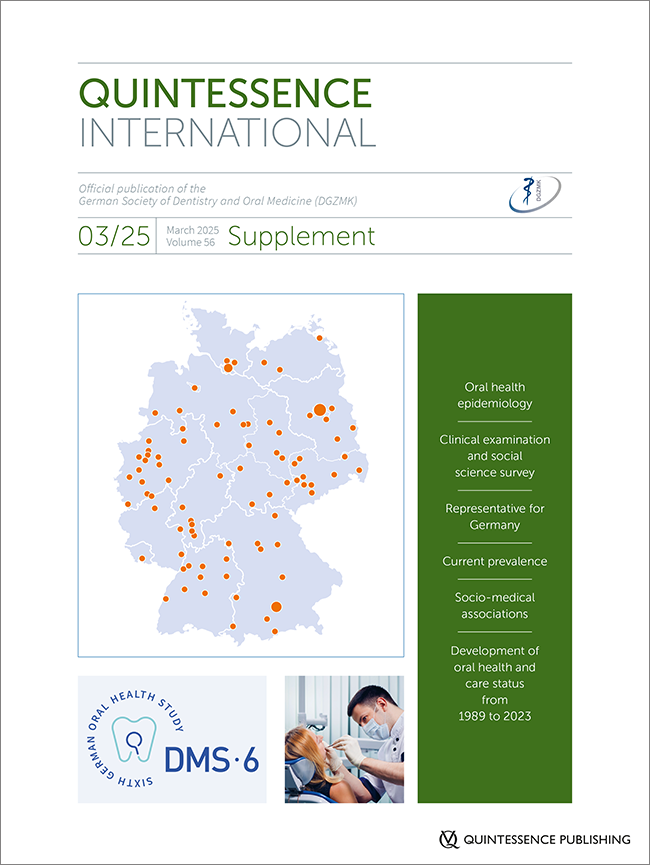
DOI: 10.3290/j.qi.b6044427, PubMed-ID: 40091716Seiten: S2-S3, Sprache: EnglischJordan, A. Rainer / Wiltfang, Jörg / Geurtsen, Werner / Heydecke, GuidoDMS • EditorialDOI: 10.3290/j.qi.b5986173, PubMed-ID: 40091717Seiten: S4-S12, Sprache: EnglischJordan, A. Rainer / Frenzel Baudisch, Nicolas / Ohm, Cristiana / Zimmermann, Fabian / Sasunna, Dominic / Cholmakow-Bodechtel, Constanze / Krämer, Marvin / Kuhr, KathrinObjectives: With the First German Oral Health Study (DMS I) in 1989, the Institut der Deutschen Zahnärzte (IDZ) laid the foundation for a population-representative socioepidemiologic monitoring of oral health and care status in Germany. The objective of the sixth wave of the survey was to update the status of oral health. Research questions: The primary questions address cross-sectional data: 1. What are the current prevalence rates of oral diseases? 2. What associations exist between oral health and other participant characteristics? The third question is based on the comparison of cross-sectional data with previous German oral health studies (trend): 3. How has the oral health and care status in Germany developed from 1989 to 2023? The last two questions require longitudinal data: 4. How do oral diseases change over the course of a lifetime? 5. What individual characteristics influence the progression of (new) oral diseases? Study design: The DMS • 6 is a combined cross-sectional and cohort study and therefore classified as an observational study. Study participants: The age groups for the cross-sectional study were selected following the World Health Organization (WHO) recommendations for oral epidemiologic studies. These include 12-year-olds as representatives for younger adolescents, 35- to 44-year-olds for younger adults, and 65- to 74-year-olds for younger seniors. An additional age group of 8- and 9-year-olds (younger children) was included to obtain information on oral health during the mixed dentition phase. In total, 3,377 study participants were included in the analyses for the cross-sectional questions (prevalences). Participant characteristics provide insights into their sociodemographic and behavioral parameters.
Schlagwörter: cross-sectional studies, dental care, dental health surveys, dentists, epidemiology, Germany, oral health, prevalence, research design
DOI: 10.3290/j.qi.b5981986, PubMed-ID: 40091718Seiten: S14-S21, Sprache: EnglischOhm, Cristiana / Kuhr, Kathrin / Zimmermann, Fabian / Frenzel Baudisch, Nicolas / Cholmakow-Bodechtel, Constanze / Krämer, Marvin / Jordan, A. RainerObjectives: The German Oral Health Studies (DMS) are nationally representative surveys on oral health in Germany, conducted approximately every 8 years since 1989. The current sixth edition of the study (DMS • 6) was planned and executed in accordance with international standards. A field institute selected from across Europe was responsible for data collection. Method and materials: For six age groups, data collection for the DMS • 6 took place across Germany from October 2022 to September 2023. Data for a seventh age group had already been collected earlier, in the spring of 2021. In addition to conducting a cross-sectional study with new participants, for the first time, a longitudinal component was included by reengaging study participants from the previous study, the Fifth German Oral Health Study (DMS V). Participation was organized via postal invitations, followed by reminder letters or personal visits if there was no response. Data collection in the field was conducted at temporarily established study centers. Data collection: The primary aim of the DMS • 6 was to assess the current oral health status, oral health behavior, and the dental care status in Germany. For this purpose, both new study participants and participants from the preceding DMS V study underwent clinical examinations and social science surveys. The clinical examinations followed a standardized protocol outlined in a manual. The social science survey was conducted in two parts: a paper and pencil interview (PAPI) completed at home and a computer-assisted personal interview (CAPI) administered immediately before the clinical examination in the study center. A non-response survey showed no systematic differences between study participants and non-participants, indicating an unbiased data basis. Quality assurance: The DMS • 6 included a comprehensive examination program supported by a multi-stage quality assurance system. This system involved pre-testing of the social science research instruments, conducting a pilot study to simulate the main study, multiple training sessions, and the calibration and certification of the dental study personnel both before and during fieldwork. This ensured a high level of data validity.
Schlagwörter: data collection, dental care, dental health surveys, dentists, DMS 6, epidemiology, surveys and questionnaires
DOI: 10.3290/j.qi.b5981988, PubMed-ID: 40091719Seiten: S22-S29, Sprache: EnglischKuhr, Kathrin / Sasunna, Dominic / Frenzel Baudisch, Nicolas / Pitchika, Vinay / Zimmermann, Fabian / Ohm, Cristiana / Jordan, A. RainerObjectives: The 6th German Oral Health Study (DMS • 6) is a combined cross-sectional and cohort study with the main objective of reporting oral diseases in Germany. Based on cross-sectional data, current prevalence estimates and trend analyses on the development of oral health and care status in Germany were conducted using representative data. Associations between oral health and further participant characteristics were examined. The aim of this article is to provide details on data handling and statistical analysis of the cross-sectional data. Sample weighting: Weighting factors were used as part of the statistical analysis to correct for deviations between the analysis set and the population structure in Germany. The objective was to make nationwide representative statements for the age groups examined in the cross-sectional component of the DMS • 6. Different types of weights were calculated: design, non-response, and calibration weights. Processing of quantitative variables: The indices and transformed variables required for data analysis were defined based on variables collected in clinical examinations and social science interviews. Dental characteristics were aggregated at the participant level. Statistical methods: For epidemiologic description, prevalence rates and means with associated 95% confidence intervals were calculated. Regression models were adjusted to estimate the strength of associations between participant characteristics of interest and oral health-related outcomes. To describe trends in the temporal development of oral health and dental care status in Germany, epidemiologic descriptions from DMS • 6 and previous studies were compared.
Schlagwörter: cross-sectional studies, data analysis, data management, dental care, dentists, DMS 6, epidemiologic studies
DOI: 10.3290/j.qi.b5986212, PubMed-ID: 40091720Seiten: S30-S39, Sprache: EnglischJordan, A. Rainer / Meyer-Lueckel, Hendrik / Kuhr, Kathrin / Sasunna, Dominic / Bekes, Katrin / Schiffner, UlrichObjectives: One goal of the 6th German Oral Health Study (DMS • 6) was to survey the caries experience and care for caries in a representative cross-sectional study across Germany. Method and materials: Using almost the same methodology as the previous studies DMS III (1997) to V (2014), data were collected on caries experience (including dmft/DMFT, root caries) in the three standard World Health Organization age groups (12-year-olds, 35- to 44-year-olds, and 65- to 74-year-olds) as well as among 8- and 9-year-olds. Results: The caries experience expressed as dmft/DMFT in 8- and 9-year-olds was 1.4 teeth, 59.9% were caries-free; the DMFT among 12-year-olds was 0.5 teeth, with 77.6% caries-free. There was a significant decrease in caries-related restorations among 35- to 44-year-olds, with DMFT being 8.3 teeth. The group of 65- to 74-year-olds had a DMFT of 17.6 teeth, which was mainly due to higher tooth retention; 5.0% were edentulous. The prevalence of root caries was 13.8% among 35- to 44-year-olds and 59.1% among 65- to 74-year-olds. Conclusions: The various oral health measures taken over recent decades seem to continue to have a positive impact in terms of reduced caries experience. Nevertheless, it appears that the maximum has been reached among 12-year-olds; however, within this group there continues to be a strong polarization of dental caries in adolescents from families with a low education status and a comparatively high treatment need for the primary teeth. The social gradient in tooth decay and tooth loss extends over the entire life span. The DMS • 6 study, being representative of the oral epidemiology of the population, shows the sustainability of successful prevention measures for caries in all age groups and education groups in Germany. At the same time, social inequalities persist. From a socio-medical perspective, it would make sense to align future prevention strategies specifically to the lifeworld of groups and communities that have not yet been reached.
Schlagwörter: cross-sectional studies, deciduous tooth, dental care, dental caries, dentists, DMS 6, root caries
DOI: 10.3290/j.qi.b5981979, PubMed-ID: 40091721Seiten: S40-S47, Sprache: EnglischEickholz, Peter / Holtfreter, Birte / Kuhr, Kathrin / Dannewitz, Bettina / Jordan, A. Rainer / Kocher, ThomasObjectives: The 6th German Oral Health Study (DMS • 6) reports on the periodontal status in population-based cohorts of younger adults (35- to 44-year-olds) and younger seniors (65- to 74-year-olds). Method and materials: Participants answered questionnaires regarding oral health behavior, and general and oral health status. Probing depth (PD), clinical attachment level (CAL), and bleeding on probing (BOP) were measured on all teeth except third molars. Number of teeth, BOP, mean PD, mean CAL, the stages of the 2018 classification of periodontal diseases, the prevalence of Community Periodontal Index (CPI), and the Centers for Disease Control and Prevention (CDC)/ American Academy of Periodontology (AAP) case definition were reported. Results: In total, 9.2%/20.6% of younger adults/younger seniors had a low education status, 25.6%/14.1% of younger adults/younger seniors were current smokers, and 2.1%/15.4% of younger adults/younger seniors had type 2 diabetes. Of all younger adults/younger seniors, 24.4%/38.7% stated that they performed interdental cleaning at least daily. The mean number of teeth in dentate younger adults/younger seniors was 26.6/20.4, of which 5.6/8.3 teeth had PD ≥ 4 mm and only 0.6/1.7 teeth had PD ≥ 6 mm. The mean number of teeth with CAL ≥ 5 mm was 1.1/3.6 in younger adults/younger seniors. Mean PD in younger adults/younger seniors was 2.1 mm/ 2.6 mm; correspondingly, mean CAL was 1.1 mm/2.4 mm. A CPI score of 4 occurred in 16.2%/42.4% of younger adults/younger seniors. In total, 13.6%/26.3% of younger adults/younger seniors were classified as having stage III periodontitis, while 3.9% and 26.4% were classified as having stage IV periodontitis according to the 2018 case classification, respectively. Conclusion: The periodontitis prevalence according to the 2018 classification (including all stages) was very high at 95.1%/85.2% in younger adults/younger seniors. In total, 31.6%/8.3% of younger adults/younger seniors were classified as stage I (ie, interdental CAL 1 to 2 mm), which, from a clinical point of view, appears to be a transitional phase between gingivitis and periodontitis, which can probably be managed with preventive rather than therapeutic measures. In younger adults and younger seniors, the prevalence of periodontitis in Germany is high, with severe periodontitis (stages III and IV) in 17.5%/52.7% of younger adults/younger seniors.
Schlagwörter: classification, dental care, dentists, DMS 6, epidemiology, prevalence, periodontitis
DOI: 10.3290/j.qi.b5981996, PubMed-ID: 40091722Seiten: S48-S58, Sprache: EnglischKocher, Thomas / Eickholz, Peter / Kuhr, Kathrin / Jordan, A. Rainer / Sasunna, Dominic / Pitchika, Vinay / Holtfreter, BirteObjectives: The objective of this study was twofold: firstly, to provide an overview of trends in periodontal status among younger adults aged 35 to 44 years and younger seniors aged 65 to 74 years between 2005 and 2023, based on data from the German Oral Health Studies (DMS); secondly, to quantify the extent to which observed differences in tooth count variables between consecutive studies can be attributed to differences in characteristics. Method and materials: The data from DMS IV (2005), DMS V (2014), and DMS • 6 (2023) were analyzed. The participants completed questionnaires concerning their oral health behaviors, and general and oral health. For this analysis, probing depths (PD) were calculated from three sites on 12 index teeth as a common denominator. The number of teeth, severity, and extent of PD and the Community Periodontal Index (CPI) were reported. Multivariate decomposition was employed to analyze differences by time. Results: The proportion of edentate younger seniors notably declined, from 23.2% to 5.4%, between 2005 and 2023. Similarly, the mean number of teeth for dentate younger seniors was 2.4 teeth higher in DMS • 6. While the mean PD remained 2.4 mm for younger adults and 2.8 mm for younger seniors, inconsistent patterns were observed for extent variables. In most cases, a decline of the extent variables was observed between DMS IV and DMS V, with a rebound at DMS • 6 for severe cases in younger seniors (with PD ≥ 6 mm). The proportion of younger adults and seniors with CPI scores of 0 to 2 increased considerably between DMS IV and DMS V, but rebounded at DMS • 6. Overall, the prevalence of these cases increased by approximately 10% points and 5% points, respectively. The majority of the observed reduction in the number of missing teeth (in younger adults) or the prevalence of having less than 20 teeth (in younger seniors) between DMS IV and DMS V and between DMS V and DMS • 6 were explained by an increase in the proportion of highly educated individuals, an increase in the proportion of those who have never smoked (only younger adults), an increase in the proportion of individuals using electric toothbrushes or interdental cleaning devices, and a reduction in the proportion of individuals with lifetime periodontal treatment. Conclusion: Over the last two decades, there has been a significant improvement in periodontal health in Germany, with the most notable enhancements occurring between DMS IV and DMS V. The prevalence of periodontal disease has decreased significantly in recent decades, largely due to the implementation of preventive measures. This underscores the importance of integrating preventive measures into dental practice as a public health strategy.
Schlagwörter: dental care, dentists, DMS 6, multivariate decomposition, number of missing teeth, periodontitis, trend analysis
DOI: 10.3290/j.qi.b5986257, PubMed-ID: 40091723Seiten: S60-S68, Sprache: EnglischWöstmann, Bernd / Samietz, Stefanie / Jordan, A. Rainer / Kuhr, Kathrin / Nitschke, Ina / Stark, HelmutObjectives: The German Oral Health Study (DMS) is a series of consecutive studies designed to assess the oral health status of adults, seniors, and children in Germany. DMS is a major program of the Institute of German Dentists (Institut der Deutschen Zahnärzte) with the aim to produce health statistics for Germany. Tooth loss, edentulism, and prosthetic care have considerable socioeconomic significance; it is the aim of this paper to report findings on these aspects. Method and materials: The survey combines interviews and clinical examinations. Previous DMS studies focused primarily on tooth loss, edentulism, and prosthetic care. In the DMS • 6 survey, the condition of removable dentures and need for adjustments were additionally recorded, as well as necessary repair measures that were grouped according to their complexity (chairside or laboratory). Results: The prevalence of edentulism decreased considerably compared to that in the Fifth German Oral Health Study (DMS V) in 2014. Among younger adults (35- to 44-year-olds), the prevalence of edentulism was negligible, with an average of 26.6 teeth present. The younger senior group (65- to 74-year-olds) had an average of 19.3 teeth; the prevalence of edentulism was 5%, which is a reduction of > 50% compared to 2014 (12.4%). Lower education status was an important prognostic factor for tooth loss. Owing to the low prevalence of edentulism in younger adults, removable dentures were not prevalent in this age group, whereas combined fixed–removable dentures were most frequently used in seniors. Regarding the type of denture, a shift towards fixed as well as implant-supported types was observed. Of the removable dentures, 50% to 60% were in a very good or good clinical condition. Problems were mainly identified with simple acrylic dentures. Nonetheless, participants’ satisfaction with removable dentures was extremely high, and the dentures were used almost continuously. Conclusion: The most important finding in this study is the continued significant decline in the prevalence of complete edentulism among seniors that suggests a further reduction in edentulism in the future with an estimate of around 4% in 2030. The shift observed in primary prosthetic care from removable to fixed prostheses as well as the increasing prevalence of implants placed are positive developments. The data revealed further compression of morbidity compared to DMS V. Complete edentulism declined, and fixed partial dentures, including implant-supported prostheses, were increasingly used. Lower education status was an important predictor for tooth loss.
Schlagwörter: dental care, dental prostheses, dentists, DMS 6, edentulous mouth, epidemiology, tooth loss
DOI: 10.3290/j.qi.b5986273, PubMed-ID: 40091724Seiten: S70-S74, Sprache: EnglischBekes, Katrin / Meyer-Lueckel, Hendrik / Jordan, A. Rainer / Kuhr, Kathrin / Schiffner, UlrichObjectives: The aim of this study was to determine the prevalence of molar incisor hypomineralization (MIH) in Germany. A secondary goal was to analyze a possible connection between MIH and caries, as well as to investigate the influence of MIH on oral health-related quality of life (OHRQoL). Method and materials: All younger adolescents (12-year-olds) from the 6th German Oral Health Study (DMS • 6) were examined for MIH according to the criteria of the European Academy of Paediatric Dentistry (EAPD). The caries experience and OHRQoL were also determined. Results: In total, 922 younger adolescents were included in the analysis. The prevalence of MIH was 15.3%; 63.3% of cases were mild forms; 8.2% of affected subjects had a caries experience. OHRQoL did not vary significantly between healthy and MIH-affected children. Conclusion: In Germany, every seventh child aged 12 years old suffers from MIH. These data on MIH in younger adolescents in Germany conform to data from regional studies; the prevalence is in the upper middle range in an international comparison.
Schlagwörter: dental care, dentists, DMS 6, epidemiology, molar hypomineralization, prevalence, quality of life
DOI: 10.3290/j.qi.b5982008, PubMed-ID: 40091725Seiten: S76-S81, Sprache: EnglischSchiffner, Ulrich / Jordan, A. Rainer / Meyer-Lueckel, Hendrik / Kuhr, Kathrin / Bekes, KatrinObjectives: In addition to caries, other dental hard tissue diseases, such as erosive wear, are gaining importance in prevention and treatment. The survey aimed to collect current data on the prevalence of erosions in younger adults and to compare these with the previous state of knowledge. Method and materials: As part of the representative 6th German Oral Health Study (DMS • 6), all teeth were assessed according to the basic erosive wear examination (BEWE). The maximum value of the findings per sextant was included in the evaluation. Results: The prevalence of erosions was found to be 43.2%. At 49.1%, men had significantly more erosions than women (37.8%). Younger adults with a high education status were affected by erosions more frequently than persons with a medium or low education status (49.2%, 37.9%, and 45.1%, respectively). Conclusion: The prevalence of erosions remains practically unchanged from the Fifth German Oral Health Study (DMS V) of 2014. However, the proportion of people at increased risk has risen sharply. The continued high prevalence of erosions combined with the increased proportion of people with a medium or high risk classification indicates that the prevention and treatment of erosive wear is a clinically relevant issue.
Schlagwörter: dental care, dentists, DMS 6, educational status, epidemiology, prevalence, risk assessment, tooth erosionn
DOI: 10.3290/j.qi.b5982011, PubMed-ID: 40091726Seiten: S82-S87, Sprache: EnglischDeinzer, Renate / Jordan, A. Rainer / Kuhr, Kathrin / Margraf-Stiksrud, JuttaObjectives: Past German Oral Health Studies (DMS) have revealed that toothbrushing patterns – a behavioral index comprising toothbrushing frequency, duration and timing – have steadily improved over the previous decades. What has not yet been investigated, however, are toothbrushing skills, ie, the ability to achieve oral cleanliness by removing all plaque deposits. Method and materials: All participants of the DMS • 6 from the age groups of 12-year-olds, 35- to 44-year-olds, and 65- to 74-year-olds were asked to brush their teeth to the best of their ability. To do so, they used their own devices or those provided. The plaque that remained after brushing was recorded using the modified Marginal Plaque Index (mMPI), expressing the percentage of segments remaining at the gingival margin that were colonized by plaque. Relationships to questionnaire data regarding demographics (age, gender, education status), toothbrushing behavior (frequency, utilization of an electric toothbrush), and selected dental treatments (professional tooth cleaning, lifetime periodontal treatment) were assessed. Results: Even following the best possible brushing, roughly half of the segments (44% to 52%) across all age groups showed persisting plaque deposits. Survey data revealed the most pronounced group differences regarding education, whereby even in the group of younger seniors with a high education status, 37% of the areas showed persisting plaque after cleaning. Conclusion: The data demonstrate that there are population-wide deficits in the ability to achieve oral cleanliness. Future prevention efforts should also focus on improving the population’s toothbrushing skills.
Schlagwörter: awareness, behavior, dental care, dental examinations, dentists, DMS 6, oral hygiene, surveys and questionnaires, toothbrushing
DOI: 10.3290/j.qi.b5982015, PubMed-ID: 40091727Seiten: S88-S94, Sprache: EnglischMargraf-Stiksrud, Jutta / Jordan, A. Rainer / Kuhr, Kathrin / Deinzer, RenateObjectives: Dietary habits have significant implications for oral health, with the consumption of sugar-rich foods being strongly associated with caries. However, additional factors must be considered to fully establish their harmful effects. These relationships are examined in three age groups of the 6th German Oral Health Study (DMS • 6). Method and materials: Dietary habits were assessed using the short form of the Marburg Sugar Index (MSI-S), which comprises six questions regarding food consumption frequencies in various contexts. Responses provide insight into the degree of cariogenic eating behavior. In addition to demographic factors (gender, education status, migration history), clinical variables such as caries experience (decayed, missing, filled teeth [DMFT] index), plaque accumulation (modified Marginal Plaque Index [mMPI]), and the number of remaining teeth were included. Results: No direct relationship between the extent of cariogenic dietary habits (MSI-S total score) and clinical variables was observed in any of the examined age groups (n = 870 younger adolescents [12-year-olds], n = 853 younger adults [35- to 44-year-olds], and n = 730 younger seniors [65- to 74-year-olds]). Gender and education status also showed no significant differences. However, 12-year-olds with a migration history exhibited higher MSI-S scores compared to those without. Analyzing extreme groups (the top and bottom 10% of MSI-S scores), systematic differences in caries experience were observed among 12-year-olds and younger seniors, and in plaque levels among younger seniors. Younger adults showed no significant differences in clinical variables, even within extreme groups. Conclusion: The MSI-S scores demonstrated that particularly cariogenic dietary habits, as opposed to more favorable ones (extreme groups), are associated with increased caries experience. This was especially evident among 12-year-olds but also observed in younger seniors. The lack of differences among adults as well as the absence of significant associations between dietary habits and clinical variables in the overall groups suggest that the impact of cariogenic diets on oral health is moderated by additional variables, such as oral hygiene practices and dental service utilization. Migration history was identified as a relevant factor among 12-year-olds. The detrimental effects of cariogenic dietary habits on oral health are most evident when analyzed in the context of additional influencing factors and stratified by target groups. Promoting oral health awareness regarding nutrition is particularly important for adolescents and seniors.
Schlagwörter: dental care, dental caries, dental plaque, dentists, diet, DMS 6, Marburg Sugar Index, nutrition
DOI: 10.3290/j.qi.b5982019, PubMed-ID: 40091728Seiten: S96-S103, Sprache: EnglischKrause, Laura / Starker, Anne / Hertrampf, Katrin / Frenzel Baudisch, Nicolas / Jordan, A. Rainer / Pitchika, Vinay / Kuhr, KathrinObjectives: Smoking is the most significant individual health risk and the leading cause of premature mortality in industrialized nations. International studies demonstrate that smoking also affects oral health adversely. This study aimed to investigate the association between smoking and oral health using population-representative data for Germany. Method and materials: The data source was the 6th German Oral Health Study (DMS • 6), conducted between 2021 and 2023. Data from a total of 2,135 individuals were included in the analyses. The distribution of sociodemographic characteristics (gender, age, education status), oral health behaviors (frequency of toothbrushing, interdental cleaning, and dental visits), and oral health-related parameters (self-assessed oral health, oral health-related quality of life, root caries, periodontitis, oral mucosal changes, and the number of teeth present) were reported separately for smoking status (daily smokers, former smokers, and never smoked). To estimate the associations between smoking status and oral health outcomes, mixed-effects regression models were employed. Results: Daily smokers exhibited worse outcomes in both self-assessed oral health parameters and clinical oral health measures compared to individuals who had never smoked. These associations persisted even after adjusting for sociodemographic factors and oral health behaviors. Similar trends were observed for former smokers compared to never smokers. Conclusion: Smoking is a well-established risk factor for poorer oral health. The findings of DMS • 6 confirm this association and are consistent with those of other national and international studies. Given the strong impact of smoking on oral health, comprehensive measures to curb smoking are essential. Evidence-based behavioral and structural preventive interventions exist to reduce tobacco consumption and promote smoking cessation. Dental offices can also contribute to tobacco prevention and cessation by providing brief counseling on the risks of smoking for both oral and general health.
Schlagwörter: dental care, dentists, DMS 6, mouth diseases, periodontitis, quality of life, smoking cessation, tobacco use
DOI: 10.3290/j.qi.b5982020, PubMed-ID: 40091729Seiten: S104-S110, Sprache: EnglischJordan, A. Rainer / Kuhr, Kathrin / Sasunna, Dominic / Rathmann, WolfgangObjectives: Epidemiologic studies have indicated a correlation between dental and cardiovascular diseases, which remains insufficiently explored. Therefore, this study aimed to compare the prevalence of common dental diseases in younger seniors (65- to 74-year-olds) with and without cardiovascular diseases. Method and materials: Participants with available self-reported data on cardiovascular diseases were selected from the cohort of the population-representative 6th German Oral Health Study (DMS • 6), in which caries, periodontitis, and tooth loss were recorded in a standardized manner. The prevalence of oral diseases was compared between participants with and without cardiovascular diseases. Results: Compared with participants without cardiovascular diseases, those with cardiovascular diseases had an average of 2.1 fewer teeth, were more frequently edentulous, and were more likely to have advanced periodontal disease (stage IV). In contrast, participants without cardiovascular disease had more fillings (mean + 1.7 teeth) than those with cardiovascular disease. Conclusion: The main cause of increased tooth loss — caries or periodontal disease — could not be clarified from the available data. In this study, the prevalence of tooth loss with oral-function limitation was higher in younger seniors with cardiovascular disease.
Schlagwörter: cardiovascular diseases, cross-sectional studies, dental care, dental caries, dentists, DMS 6, epidemiology, oral health, risk factors
DOI: 10.3290/j.qi.b5982021, PubMed-ID: 40091730Seiten: S112-S119, Sprache: EnglischSamietz, Stefanie / Wöstmann, Bernd / Kuhr, Kathrin / Jordan, A. Rainer / Stark, Helmut / Nitschke, InaObjectives: Oral health plays a central role in overall well-being, including in the elderly. The demographic transition and its effects are resulting in a higher proportion of older people, both with and without care requirements. This paper provides an overview of the dental situation of the elderly from the 6th German Oral Health Study (DMS • 6). Method and materials: DMS • 6 is a population-representative oral epidemiologic study that surveys oral health in Germany. Data from 797 younger seniors aged 65 to 74 were collected by calibrated examiners. The methodology remains largely consistent with that of the previous studies. Results: Among the younger seniors (65- to 74-year-olds), edentulism has more than halved to 5.0% compared to the Fifth German Oral Health Study (DMS V) (12.4% in 2014). The mean number of missing teeth (8.6) decreased further, compared to DMS IV (14.1) and DMS V (11.1). At 18.8 teeth, the FST Index (number of filled or sound teeth) has shown improvement compared to the previous studies (DMS IV, 13.6; DMS V, 16.4). The root caries (59.1%) increased compared to DMS IV (28.0%). Caries experience (decayed, missing, filled teeth [DMFT]: 17.6), in contrast, hardly changed from DMS V (17.7). Half of 65- to 74-year-olds were diagnosed with moderate periodontitis (49.4%) and almost a third (30.4%) with severe periodontitis. In younger seniors with care requirements, therapeutic capability was greatly reduced for almost half (47.4%) and oral hygiene ability for one fifth (18.5%). Conclusion: The prevalence of tooth loss and edentulism among younger seniors in Germany continues to decline. Due to further morbidity compression, the challenges of dental treatment lie in the continuous treatment of younger seniors to prepare them for older stages of life.
Schlagwörter: care needs, dental care, dental care for persons with disabilities, dental caries, dentists, DMS 6, epidemiology, geriatric dentistry, oral health
DOI: 10.3290/j.qi.b5981982, PubMed-ID: 40091731Seiten: S120-S125, Sprache: EnglischAarabi, Ghazal / Schenk, Liane / Kuhr, Kathrin / Borof, Katrin / Jordan, A. Rainer / Lieske, BeritObjectives: As part of the 6th German Oral Health Study (DMS • 6), the migration history of the study participants was determined at the population level for the first time. Method and materials: The evaluation and presentation of migration-related indicators, oral health behavior, and oral diseases were carried out separately for 12-year-olds, 35- to 44-year-olds, and 65- to 74-year-olds. Results: When considering the prevalence of disease and care, differences were found between people with and without migration history in all three age groups. The first group had higher prevalences of oral diseases as well as a more complaint-oriented utilization of dental services. Conclusion: The data on the prevalence of oral diseases, oral health behavior, and dental service utilization provide evidence that people with migration history do not seem to benefit in the same way from group and individual prophylaxis services as people without migration history.
Schlagwörter: behavior, dental care, dentists, DMS 6, human migration, oral health
DOI: 10.3290/j.qi.b5982024, PubMed-ID: 40091732Seiten: S126-S134, Sprache: EnglischLieske, Berit / Schenk, Liane / Kuhr, Kathrin / Pitchika, Vinay / Borof, Katrin / Jordan, A. Rainer / Aarabi, GhazalObjectives: Studies have demonstrated a significant association between migration history and oral health. Even after adjusting for confounders, migration history remains an independent risk factor for poorer oral health. As part of the 6th German Oral Health Study (DMS • 6), disease and care prevalence among individuals with migration history was surveyed at the population level. This article aims to assess the relationship between migration history, education status, and oral health. Method and materials: The analyses of the relationship between migration history and various oral health outcomes were conducted separately for younger adolescents (12-year-olds), adults (20-year-olds, 35- to 44-year-olds, 43- to 52-year-olds), and seniors (65- to 74-year-olds, 73- to 82-year-olds). Results: A significant association between migration history and poorer oral health outcomes, as well as less favorable oral health behaviors, was observed across all age groups. After adjusting for age, gender, and education, individuals with migration history exhibited higher levels of plaque, more bleeding sites, a higher prevalence of decayed teeth, insufficient tooth brushing frequency, and complaint-oriented dental service utilization. Conclusion: Previous studies have consistently identified education as a risk factor for poorer oral health. In the present study, even after adjusting for education status in multivariate models, the association between migration history and oral health outcomes remained significant. This finding underscores migration history as an independent risk factor for poorer oral health outcomes. This is the first large-scale cohort study in Germany to analyze the relationship between migration history and multiple oral health outcomes across different age groups. Future research should focus on uncovering migration-related factors, health literacy, and health behaviors to better explain the observed differences and improve oral health for migrant populations.
Schlagwörter: cross-sectional studies, dental care, dentists, DMS 6, education, epidemiology, health behavior, human migration, oral health