2019-1
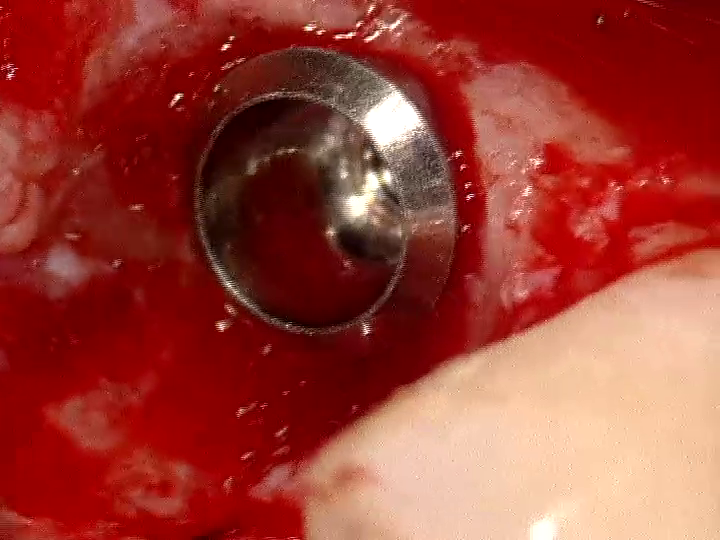
Seiten: 6-21, Sprache: EnglischBuser, Daniel / Chappuis, Vivianne / Janner, Simone F. M. / Belser, Urs C.Implant placement post single tooth extraction in the esthetic zone is an important and frequent indication for implant therapy. Today, the clinician can choose from four different treatment approaches for the timing of implant placement. The decision for the most appropriate treatment plan should be based on a thorough clinical and radiographic examination and well-defined selection criteria. Early implant placement after soft tissue healing is one of the treatment options available. This approach is applied by our team in the case of a thin bone wall phenotype ( 1 mm) or a missing facial bone wall at the extraction site, and sufficient bone volume available in the palato-apical area to allow good primary stability of the implant. The surgical procedures include a flapless tooth extraction, a 4-to-8 week soft tissue healing period, implant placement in the correct 3-dimensional position, a simultaneous contour augmentation on the facial aspect with the GBR technique using a 2-layer composite graft with locally harvested autologous bone chips and a low-substitution bone filler, application of a double-layer collagen membrane, and a tension-free primary wound closure. Following 8 weeks of healing, the implant site is reopened with a punch technique, and the implant can be restored with a screw-retained single crown. The rationale for this surgical approach is presented including inclusion criteria, surgical procedures, case reports and long-term documentation.
Schlagwörter: Implant placement post extraction, immediate implant placement, early implant placement, late implant placement, GBR technique, contour augmentation, 2-layer composite graft
International Journal of Periodontics & Restorative Dentistry, 6/2017
DOI: 10.11607/prd.3163, PubMed-ID: 29023610Seiten: 808-817, Sprache: EnglischJurczyk, Karolina / Belser, Urs C. / Sculean, AntonIn cases of single missing teeth, implant rehabilitation is generally the preferred treatment option. However, obtaining pleasing esthetic results in the anterior maxillary region and maintaining or rebuilding peri-implant papillae remain challenging tasks. The loss of papillae may cause not just functional but also phonetic and esthetic problems. There is scarce information on the reliability of surgical approaches concerning the peri-implant papilla. The purpose of this case report is to present a modified prosthetic-surgical technique to enhance the convex facial contour of the peri-implant mucosa and volume and height of papillary tissue in an esthetically highly demanding patient.
The International Journal of Oral & Maxillofacial Implants, 2/2017
DOI: 10.11607/jomi.5295, PubMed-ID: 28291853Seiten: 350-355, Sprache: EnglischPark, Ji-Man / Baek, Chang-Hyun / Heo, Seong-Joo / Kim, Seong-Kyun / Koak, Jai-Young / Kim, Shin-Koo / Belser, Urs C.Purpose: The aim of this study was to compare the loosening of interchangeable one-piece abutments connected to internal-connection-type implants after cyclic loading.
Materials and Methods: Four implant abutment groups (n = 7 in each group) with Straumann tissue-level implants were assessed: Straumann solid abutment (group S), Southern Implants solid abutment (group SI), Implant Direct straight abutment (group ID), and Blue Sky Bio regular platform abutment (group BSB). The implant was firmly held in a special jig to ensure fixation. Abutment screws were tightened to manufacturers' recommended torque with a digital torque gauge. The hemispherical loading members were fabricated for the load cell of a universal testing machine to evenly distribute the force on the specimens and to fulfill the ISO 14801:2007 standard. A cyclic loading of 25 N at 30 degrees to the implant's long axis was applied for a duty of a half million cycles. Tightening torques were measured prior to the loading. Removal torques were measured after cyclic loading. The data were analyzed with one-way analysis of variance (ANOVA), and the significance level was set at P .05.
Results: The mean removal torques after cyclic loading were 34.0 ± 1.1 Ncm (group S), 25.0 ± 1.5 Ncm (group SI), 23.9 ± 2.1 Ncm (group ID), and 27.9 ± 1.3 Ncm (group BSB). Removal torques of each group were statistically different in the order of group S > group BSB > groups SI and ID (P .05). The mean reduction rates were -2.9% ± 3.2% (group S), -21.9% ± 4.8% (group SI), -20.2% ± 7.2% (group ID), and -6.9% ± 4.3% (group BSB) after a half million cycles, respectively. Reduction rates of groups S and BSB were statistically lower than those of groups SI and ID (P .01). The standard deviation of group S was lower than group BSB.
Conclusion: The removal torque of the original Straumann abutment was significantly higher than those of the copy abutments. The reduction rate of the groups S and BSB abutments was lower than those of the other copy abutments.
Schlagwörter: cyclic loading, implant abutment, implant-abutment stability, internal-connection-type implant, removal torque, screw loosening
International Journal of Esthetic Dentistry (EN), 4/2015
PubMed-ID: 26794049Seiten: 522-532, Sprache: EnglischMoráguez, Osvaldo D. / Vailati, Francesca / Belser, Urs C.This two-part case presentation describes the prosthetic challenge of managing complications in a 50-yearold female patient after inadequate esthetic risk assessment, treatment planning, and implant placement in the anterior maxilla. In Part I, the clinical situation was described, and different restorative solutions were proposed to correct the extreme facial inclination of the implants, excluding major surgical procedures, namely implant removal. In Part II, different prosthetic options are discussed, and the final treatment is revealed. A noninvasive treatment protocol was applied to transform a severely compromised postsurgical situation into an esthetically acceptable result. An unconventional prosthesis design was implemented, including the use of ceramic veneers bonded to the CAD/ CAM -generated screw-retained zirconia- based fixed dental prosthesis (FDP), to correct major axis-related problems and spatial discrepancies.
International Journal of Esthetic Dentistry (DE), 4/2015
Seiten: 506-516, Sprache: DeutschMoráguez, Osvaldo D. / Vailati, Francesca / Belser, Urs C.Teil II: Fallbericht und DiskussionIn diesem zweiteiligen Fallbericht wird die Problematik des prothetischen Komplikationsmanagements beschrieben, nachdem bei einer 50-jährigen Patientin eine unzureichende ästhetische Risikoanalyse, Behandlungsplanung und Implantatsetzung im Oberkiefer-Frontzahnbereich vorgenommen worden war. Im ersten Teil wurde die klinische Ausgangssituation geschildert und verschiedene restaurative Lösungen zur Korrektur der extremen Labialneigung der Implantate vorgeschlagen. Größere chirurgische Maßnahmen, insbesondere die Implantatentfernung, wurden dabei ausgeschlossen. Im zweiten Teil werden unterschiedliche prothetische Optionen diskutiert und die definitive Behandlung vorgestellt. Letztlich wurde ein nichtinvasives Vorgehen gewählt, um die extrem ungünstige Situation nach der Implantation zu einem ästhetisch akzeptablen Ergebnis zu führen. Hierzu diente eine unkonventionelle Restaurationsgestaltung mit Keramikveneers, die adhäsiv auf einer CAD/CAMgefertigten, verschraubten Brücke mit Zirkonoxidgerüst befestigt wurden. Die Hauptschwierigkeiten mit der Implantatachse und den Platzproblemen konnten damit gelöst werden.
International Journal of Esthetic Dentistry (DE), 3/2015
Seiten: 340-346, Sprache: DeutschMoráguez, Osvaldo D. / Vailati, Francesca / Belser, Urs C.Teil I: Fallbericht und BehandlungsoptionenIn diesem zweiteiligen Fallbericht werden die prothetischen Herausforderungen beschrieben, die beim Komplikationsmanagement nach einer unzureichenden ästhetischen Risikobewertung, Behandlungsplanung und Implantatpositionierung im Oberkiefer-Frontzahnbereich entstehen. Im ersten Teil wird eine 50-jährige Patientin vorgestellt, die nach einer unsachgemäß ausgeführten Sofortimplantation überwiesen wurde. Verschiedene restaurative Behandlungsoptionen werden vorgeschlagen, die ohne umfangreiche chirurgische Maßnahmen auskommen. Im zweiten Teil dieses Berichts werden die Vor- und Nachteile der verschiedenen prothetischen Optionen diskutiert und die gewählte Behandlung vorgestellt. Ziel dieses ersten Teils ist es, die Wichtigkeit einer angemessenen Behandlungsplanung herauszustellen, denn die Korrektur eines ästhetischen Implantatmisserfolgs führt regelmäßig zu einem eingeschränkten Ergebnis verglichen mit dem, was in der Ausgangssituation möglich gewesen wäre.
International Journal of Esthetic Dentistry (EN), 3/2015
PubMed-ID: 26171441Seiten: 368-373, Sprache: EnglischMoráguez, Osvaldo D. / Vailati, Francesca / Belser, Urs C.This two-part case presentation describes the prosthetic challenge of managing complications after inadequate esthetic risk assessment, treatment planning, and implant positioning in the anterior maxilla. Here, the case report of a 50-year-old woman, referred after inappropriate execution of immediate implant placement, is presented. Different restorative treatment alternatives are proposed, excluding major surgical procedures. In the next part of the article, the advantages and shortcomings of the various prosthetic options will be discussed and the selected treatment revealed. The aim of this part of the article is to illustrate the importance of treatment planning, emphasizing that the correction of esthetic implant failures consistently leads to compromised results when compared to what could have been achieved first time round.
International Journal of Periodontics & Restorative Dentistry, 5/2014
DOI: 10.11607/prd.1808, PubMed-ID: 25171038Seiten: 672-679, Sprache: EnglischGonzález-Martín, Oscar / Veltri, Mario / Moráguez, Osvaldo / Belser, Urs C.The aim of this study was to describe a technique for the assessment of soft tissue volumetric and profilometric changes. The technique has been applied at the alveolar contour of mild to moderate horizontal ridge defects after soft tissue augmentation at pontic sites. A quantitative three-dimensional (3D) analysis based on laser scanning was used for the measurement of volume gain and horizontal changes of alveolar profile 5 months after a subepithelial connective tissue graft using a pouch approach in five patients. All the surgical sites healed uneventfully. A mean soft tissue volume increase of 35.9 mm3 was measured 5 months after the grafting procedure. The linear measurements showed that, in the area where the augmentation was performed, the distance between the preoperative vestibular profile and the postoperative one ranged from 0.16 to 2 mm. The described quantitative measurements based on 3D laser scanning appear to be an effective method for assessment of soft tissue changes in future studies. Additionally, within the limitation of a small sample size, the present data suggest that the investigated surgical technique can be considered when corrections of mild to moderate alveolar horizontal ridge atrophies at maxillary lateral incisor edentulous gaps are necessary.
The International Journal of Oral & Maxillofacial Implants, 5/2014
DOI: 10.11607/jomi.3068, PubMed-ID: 25216137Seiten: 1114-1122, Sprache: EnglischCaram, Santiago J. / Huynh-Ba, Guy / Schoolfield, John D. / Jones, Archie A. / Cochran, David L. / Belser, Urs C.Purpose: The purpose of this experimental study was to analyze radiographically in a dog model how different implant-abutment interface configurations influence alveolar crestal bone changes.
Materials and Methods: Six different experimental implant-abutment connections were evaluated in six mixed-breed dogs. The following parameters were tested: absence of microgap, microgap proximal to bone crest, and microgap distant from bone crest. In addition, two different cervical abutment profiles, one straight and one featuring a supracrestal concavity, were evaluated. Implants were based on a cylindrical full-body screw design and made from coldworked grade IV commercially pure titanium. The diameter (at thread tips) measured 4.1 mm, whereas the inner diameter was 3.5 mm. Standardized periapical digital radiographs were obtained for comparative analysis at baseline and at 3, 4, 5, 6, 7, 8, and 9 months after implant placement. Radiographs were randomized and calibrated for linear measurements. For statistical analysis, mixed-model repeated-measures analysis of variance was used.
Results: All implants integrated successfully and remained stable during the entire period of the study. Radiographically, when comparing groups with straight profiles, crestal bone remodeling in group C (one-piece design) was significantly less than in group A (matching diameters) and B (nonmatching diameters). In fact, implant group C showed the least crestal bone remodeling of all groups. When comparing groups with a concave profile but different microgap configurations, all three designs demonstrated bone loss with no significant differences among the three groups.
Conclusion: A nonsubmerged one-piece implant design demonstrated the least amount of bone remodeling of all groups. Implant-abutment connections with a concave profile established crestal bone levels immediately apical to the concavity regardless of the microgap variable.
Schlagwörter: alveolar bone loss/etiology, dental implants, horizontal offset, platform switching, supracrestal concavity
International Journal of Periodontics & Restorative Dentistry, 4/2013
DOI: 10.11607/prd.1268, PubMed-ID: 23820704Seiten: 447-455, Sprache: EnglischWittneben, Julia-Gabriela / Buser, Daniel / Belser, Urs C. / Brägger, UrsAn optimal esthetic implant restoration is a combination of a visually pleasing prosthesis and surrounding peri-implant soft tissue architecture. This article introduces a clinical method, the dynamic compression technique, of conditioning soft tissues around bone-level implants with provisional restorations in the esthetic zone. The technique has several goals: to establish an adequate emergence profile; to recreate a balanced mucosa course and level in harmony with the gingiva of the adjacent teeth, including papilla height/width, localization of the mucosal zenith and the tissue profile's triangular shape; as well as to establish an accurate proximal contact area with the adjacent tooth/implant crown.