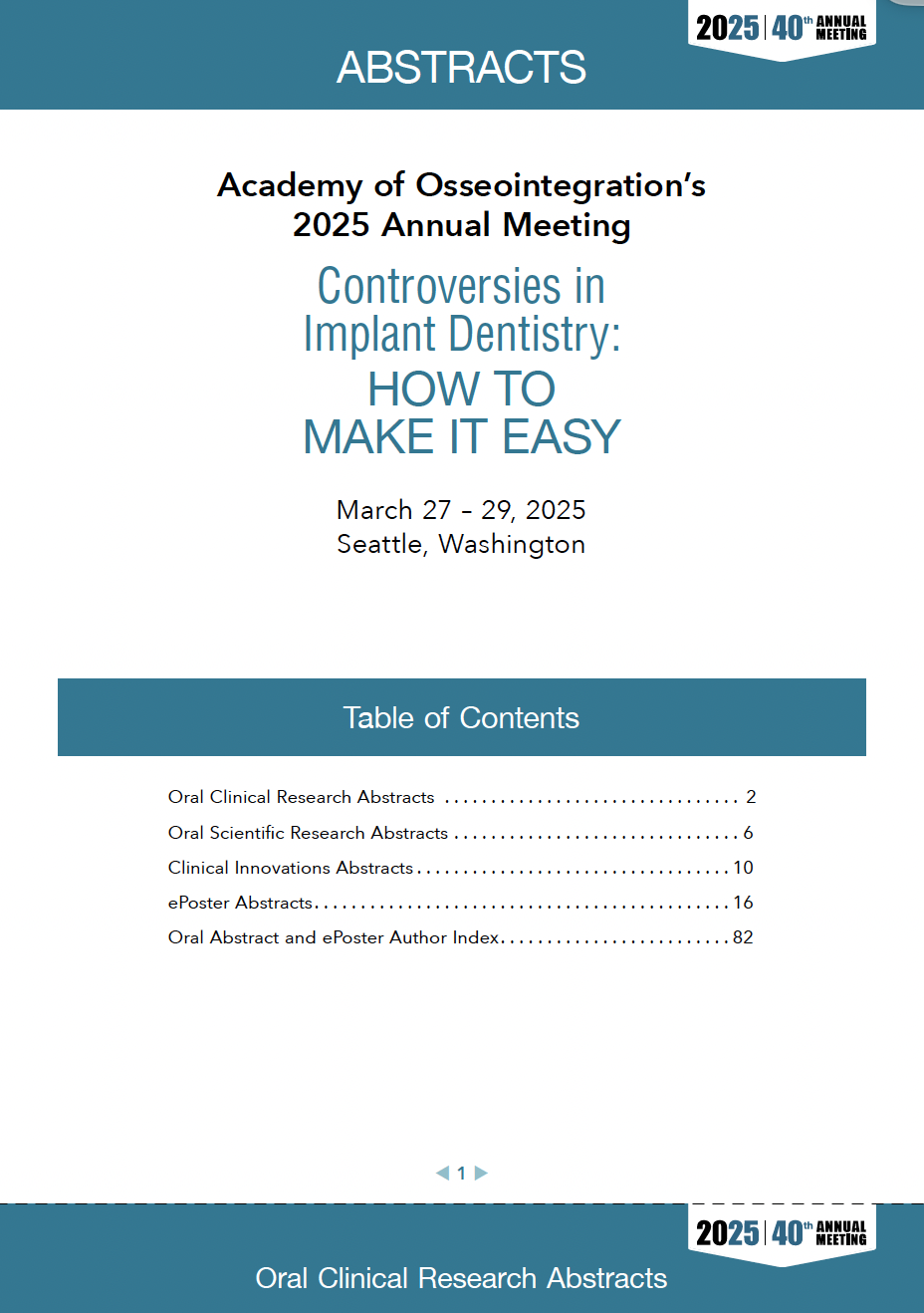
Open Access Supplement Online OnlySprache: EnglischThe consensus papers from the AO/AAP Consensus on Prevention and Management of Peri-implant Diseases and Conditions were published across multiple journals, and all articles listed in this TOC link to their respective journal sites.
Open Access Supplement Online OnlyDOI: 10.11607/jomi.2025suppl1Seiten: s1-s48, Sprache: EnglischBarootchi, Shayan / Monje, Alberto / Sabri, Hamoun / Rosen, Paul S. / Wang, Hom-LayPurpose: Reports on the occurrence of peri-implant diseases date back nearly two decades. Despite the attempts taken toward the management of this disease, the literature still lacks a common remedy for predictable treatment. This best evidence consensus review was conducted in preparation for the joint consensus between the American Academy of Periodontology (AAP) and the Academy of Osseointegration (AO) to systematically analyze the clinical research in the field of surgical reconstructive therapy for peri-implantitis. Materials and Methods: A detailed systematic search was conducted to identify eligible clinical research reporting the outcomes of surgical reconstructive therapy for periimplantitis. The retrieved nonrandomized studies were analyzed descriptively, while the data from randomized control trials (RCTs) were fit to a series of mixed models that analyzed the individual components of the study arms and rendered treatments for the outcomes of probing pocket depth (PPD) reduction, radiographic marginal bone level (Rx MBL) gain, reduction in bleeding on probing (BoP) and suppuration (SUP), as well as mucosal recession (MREC). Results: A total of 18 reports on RCTs were eligible for quantitative assessment (635 patients, 687 implants). The results indicated that surgical reconstructive approaches for peri-implantitis (based on 319 patients and 345 implants), when compared to a nonreconstructive treatment modality (ie, open flap debridement alone based on 316 patients and 342 implants), was effective in reducing PPD, minimizing MREC, as well as increasing Rx MBL gain. However, there was no additional benefit from employing a reconstructive approach regarding the outcomes of BoP and SUP reduction. Several other baseline covariates such as site (initial PPD, MBL, and BoP) and systemic factors (eg, smoking) were also found to significantly impact the therapeutic outcomes. Mechanical decontamination methods as well as individual components of the augmentation approach were also found to significantly affect the outcomes. Conclusions: Within the limitations of this study, it was demonstrated that the surgical treatment of infrabony peri-implantitis defects can lead to PPD reduction, MREC reduction, and Rx MBL gain and was found to be superior to nonreconstructive treatment. However, there were no significant differences between the two modalities of therapy for the outcomes of BoP and SUP. Reconstructive therapy may provide a suitable approach for managing peri-implantitis–related infrabony defects.
Schlagwörter: alveolar bone grafting, dental implants, evidence-based dentistry, network meta-analysis, peri-implantitis
Open Access Supplement Online OnlyDOI: 10.11607/jomi.2025suppl2Seiten: s49-s72, Sprache: EnglischLin, Guo-Hao / Chambrone, Leandro / Rajendran, Yogalakshmi / Avila-Ortiz, GustavoPurpose: To assess whether adjunctive treatment modalities offer therapeutic advantages when used in combination with peri-implant debridement—defined as supra- and/or submarginal debridement using manual, sonic, and/or ultrasonic instrumentation—for the treatment of peri-implant mucositis. Materials and Methods: Relevant articles published in English between January 1980 and October 2023 were searched. Clinical trials involving ≥ 10 patients diagnosed with peri-implant mucositis and treated with debridement alone versus debridement plus an adjunctive treatment were included. Data were extracted and meta-analyses were performed to investigate the effect of different therapeutic approaches on several outcomes of interest (ie, pocket depth [PD] and bleeding on probing [BoP] reduction as well as complete disease resolution). Results: A total of 25 articles were selected, of which 19 were included in the meta-analyses. Peri-implant debridement generally resulted in PD and BoP reduction. For studies including nonsmokers or patients with unclear smoking status, outcomes of individual studies revealed that the use of certain probiotics, such as Lactobacillus reuteri strains, may modestly reduce BoP in the short term. For studies exclusively involving smokers or users of vapes/ electronic cigarettes, the clinical benefits of adjunctive therapy were negligible. Complete disease resolution was not consistently achieved regardless of the treatment modality. Conclusions: Peri-implant debridement as a monotherapy for the treatment of peri-implant mucositis generally results in clinical improvements in terms of PD and BoP reduction. The use of adjunctive treatment modalities does not appear to provide a clinically significant additional therapeutic benefit compared to debridement alone, independent of the patient’s smoking status. Complete peri-implant mucositis resolution is an elusive outcome.
Schlagwörter: decontamination, dental implants, meta-analysis, osseointegration, systematic review
Open Access Supplement Online OnlyDOI: 10.11607/jomi.2025suppl3Seiten: s73-s90, Sprache: EnglischSaleh, Muhammad H. A. / Misch, Craig / Alrmali, Abdusalam / Neiva, RodrigoPurpose: To estimate and compare the effect of two different nonreconstructive surgical techniques for treating periimplantitis. Materials and Methods: An electronic search was performed in PubMed, Web of Science, Embase, Scopus, Ovid Medline, and the Cochrane Library of the Cochrane Collaboration (CENTRAL) for articles published until September 2023. Studies evaluating surgical nonreconstructive techniques for the treatment of peri-implantitis were included. The primary outcomes were changes in pocket probing depth (PPD) and bleeding on probing (BoP). Secondary outcomes included marginal bone levels (MBLs) and plaque index (PI) changes. Meta-analysis and meta-regression were performed. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was used to determine the quality of evidence. Results were grouped according to their treatment techniques: (1) flap surgeries and (2) osseous resective surgeries (nonreconstructive). Results: The final stage of screening included 15 clinical trials. At 12 months, the flap group had a mean PPD reduction of 1.27 mm (95% CI: 0.67–1.87; I2 = 95.9%), and the osseous resective group had a PPD reduction of 1.88 mm (95% CI: 1.39–2.37; I2 = 97.1%), showing no significant differences (P = .119). Regarding BoP, there were no significant differences between the two techniques at 3, 6, or 12 months. For MBL, at 12 months, the flap group showed less bone loss than the osseous resective group (mean difference = 0.73 mm; P < .001). Conclusions: Both nonreconstructive surgical interventions were effective in managing peri-implantitis. Moderate-quality evidence suggested that flap surgeries may provide a slight advantage in maintaining MBLs compared to osseous resective surgery.
Schlagwörter: dental implants, peri-implantitis, systematic review, therapy
Open Access Supplement Online OnlyDOI: 10.11607/ jomi.2025suppl4Seiten: s91-s160, Sprache: EnglischRavidà, Andrea / Dias, Debora R. / Lemke, Robert / Rosen, Paul S. / Bertolini, Martinna M.Purpose: To evaluate the nonclinical evidence concerning the efficacy of different decontamination methods in facilitating reosseointegration, eliminating biofilm from implant surfaces, and their potential to induce adverse surface modifications and release of material remnants. Materials and Methods: Systematic electronic and manual searches were conducted to identify publications involving animal or human block biopsies, ex vivo/in situ studies, and in vitro studies. Mechanical, chemical, and electrolytic methods for implant decontamination were presented in a descriptive analysis. Results: A total of 121 studies were included, namely 46 involving animal/human biopsies, 39 ex vivo/in situ experiments, and 36 in vitro investigations. No modality demonstrated significant superiority in terms of reosseointegration outcomes. Ex vivo, in situ, and in vitro studies reported that greater biofilm removal from implant surfaces occurred with polyetheretherketone (PEEK) ultrasonic tips, air-powder abrasive (APA), erbium: yttrium-aluminum-garnet (Er:YAG) laser, and electrolytic cleaning. Minimal surface alterations were noted with soaked cotton pellets, APA, specific settings of Er:YAG laser, erbium, chromium: yttrium-scandium-gallium-garnet (Er,Cr:YSGG) laser, electrolytic treatment, and cold atmospheric plasma. Titanium or stainless steel curettes, ultrasonic tips, titanium brushes, and implantoplasty induced significant surface alterations and peak flattening of implant threads. Plastic and carbon curettes as well as PEEK ultrasonic tips and APA left material remnants. Conclusions: Implant reosseointegration is possible following appropriate surface decontamination. Application of Er:YAG laser, electrolytic cleaning, and APA stand out as the methods that most closely embody the ideal characteristics of an effective decontamination protocol.
Schlagwörter: dental implants, disinfection, efficiency, lasers, osseointegration, peri-implantitis