International Journal of Periodontics & Restorative Dentistry, Pre-Print
DOI: 10.11607/prd.7624Juli 11, 2025,Seiten: 1-32, Sprache: EnglischChang, Jae W. / Bi, Jiarui / Min, Seiko / Gräfin von Krockow, Nadine / Weigl, PaulBackground: Immediate implant placement has become increasingly prevalent in clinical practice, and accurate assessment of placement quality is crucial to ensure successful outcomes. Bone-to-implant contact (BIC) is one of the critical determinants of primary stability following implantation. However, its correlation to the implant stability quotient (ISQ) is uncertain. This study aims to determine the relationship between ISQ measurements and BIC in immediately placed implants. Materials and Methods: An atraumatic extraction followed by immediate implant placements were performed on 33 teeth in seven human cadaver heads. The implant ISQ values were measured in four directions: buccal, lingual, mesial, and distal. The cadaver heads were imaged using cone-beam computed tomography (CBCT) to determine the linear BICs in the corresponding directions. Results: Among the twenty-eight implants analyzed, no correlations were observed between directional BICs and the corresponding ISQ values. ISQ measurements did not significantly differ between maxillary and mandibular implants, nor among different anatomical locations. Additionally, when solid contact was present at the implant shoulder, the ISQ values remained stable despite the absence of apical BIC. Conclusion: ISQ values alone appear to be poor predictors of BIC in immediately placed implants. Therefore, ISQ measurements should be interpreted alongside other assessment methods to more accurately evaluate implant stability.
Schlagwörter: Immediate implant placement, Bone-to-implant contact, Implant stability quotient
The International Journal of Oral & Maxillofacial Implants, 2/2025
DOI: 10.11607/jomi.11039, PubMed-ID: 38941168Seiten: 207-217, Sprache: EnglischGehrke, Peter / Pietruska, Maria Julia / Korth, Anissa / Schöttler, Tanja / Jenatschke, Rafaela / Fischer, Carsten / Sader, Robert / Weigl, PaulPurpose: To retrospectively evaluate the long-term clinical, technical, biologic, and esthetic outcomes of implant-supported single zirconia crowns (ISCs) intraorally cemented to titanium-base (Ti-base) hybrid abutments up to 16 years after placement. Materials and Methods: A total of 63 ISCs were evaluated in 36 patients at two different private practices.Original Ti-bases were selected, and zirconia (Zr) mesostructures and Zr crowns were designed using CAD/CAM software and then milled from partially stabilized Zr blocks. After the mesostructures were cemented extraorally onto the Ti-bases, the Zr crowns were intraorally luted to the hybrid abutments. The Ti-base ISC restorations were followed for up to 16 years, and their clinical, biologic, and esthetic outcomes were recorded at distinct time points at 3-year intervals: October 2019 (T1) and October 2022 (T2). Results: A total of 36 patients (18 men, 18 women) received 32 ISCs in the anterior region and 31 ISCs in the posterior region of the maxilla and mandible. The mean follow-up of the Ti-base ISCs was 6.93 ± 2.60 years. The mean follow-up of the implants amounted to 8.11 ± 3.26 years. No implants were lost during follow-up, resulting in a cumulative implant survival rate of 100%. Abutment screw loosening was observed in two ISCs after 1 year of function. The overall cumulative restorative survival rate of the Ti-base restorations was 96.83%. At the T2 follow up, 24% of the ISCs exhibited an increase in probing depth (PD) despite maintaining clinically healthy peri-implant tissue. An 11% increase in bleeding on probing (BoP) and a 3.17% decrease in the plaque index (PI) were recorded. Despite spectrophotometrically measured ΔE values indicating visible discoloration of some restorations and their peri-implant soft tissue, a low incidence of esthetic complications was observed with an average pink and white esthetic score (PES/WES) of ≥ 12. No correlation was found between PES (R = –0.25; P = .27) and WES (R = –0.18; P = .43) scores and digital shade determination. Conclusions: The results indicate satisfactory clinical outcomes for intraorally cemented ISCs supported by Ti-base hybrid abutments. An overall esthetic superiority of Ti-base ISCs could not be confirmed.
Schlagwörter: retrospective trial, titanium base, zirconia, two-piece hybrid abutment, implant-supported single crown.
International Journal of Oral Implantology, 2/2025
Seiten: 135-144, Sprache: EnglischGiulini, Mika / Kassem, Nizar / Schwarz, Frank / Weigl, Paul / Schwiertz, Andreas / Sader, Robert / Lorenz, JonasPurpose: Ceramic implants are gradually becoming an alternative to standard titanium implants; however, there is still a lack of scientific data on the former. Thus, the present study was conducted to assess the clinical and microbiological performance of a two-piece ceramic implant system after a mean follow-up period of 2 years. Materials and methods: A total of 17 patients from a collective of 21 from a private dental practice that met the inclusion criteria received 32 two-piece ceramic implants (CERALOG, BioHorizons Camlog, Basel, Switzerland). The implants were restored with single crowns or three-unit fixed partial dentures. Implant survival, probing pocket depth, bleeding on probing, mucosal recession/creeping, keratinised mucosa width, Papilla Presence Index, peri-implant marginal bone level and microbiological contamination were evaluated after a mean loading period of 24 months (range 12 to 41 months). Results: All implants survived and were suitable for retaining prostheses. Probing pocket depth of 3.7 mm ± 0.7 mm and bleeding on probing on 84% of implants were recorded. Sufficient keratinised mucosa width (6.6 ± 2.9 mm) was observed with no mucosal recession/creeping. The Papilla Presence Index varied between 0 and 4 with a mean value of 1.70 ± 1.07. Mean marginal bone loss was 1.2 ± 0.9 mm. Microbiological investigation revealed no statistically significant difference in the total number of bacteria between teeth and implants (P = 0.2278); however, probing pocket depth > 4 mm proved to be a significant predictor for an increased number of bacteria (P 0.001). Conclusion: Within the limitations of the present study, the investigated two-piece ceramic implant system achieved fully satisfying functional and microbiological results. Interpretation of the clinical, radiographic and microbiological results cannot support the hypothesis that ceramic implants are less affected by peri-implant disease.
Schlagwörter: ceramic implants, microbiological test, two-piece ceramic implants, zirconia implants
The authors declare there are no conflicts of interest relating to this study.
The International Journal of Prosthodontics, 1/2025
DOI: 10.11607/ijp.8719, PubMed-ID: 38408133Seiten: 27-34, Sprache: EnglischLorenz, Jonas / Blume, Maximilian / Schwarz, Frank / Weigl, Paul / Ghanaati, Shahram / Sader, Rober A.Purpose: To investigate the effect of immediate provisionalization of single-tooth implants at healed sites for peri-implant soft-tissue conditions, focusing on papilla formation around single implants. Materials and Methods: In total, 12 patients received a total of 12 implants in the incisor, canine, or premolar region of the maxilla or mandible at healed sites with immediate chairside provisionalization. After 4 months, the temporary crown was replaced with the permanent crown. After 40 ± 13.1 months, clinical follow-up was conducted, assessing probing pocket depth (PPD), bleeding on probing (BoP), mucosal recession (MR), and width of keratinized mucosa (KM). Papilla index (PI) was determined immediately after implant placement (t0), before removing the temporary crown (t1), 4 weeks after delivery of the definitive crown (t2), and at the final follow-up examination (t3) to evaluate papilla formation and its change over time. Results: None of the implants were lost. The mean PPD was 2.5 ± 0.39 mm, and BoP of 25% and 3.5 mm of KM were observed at the final follow-up. No implants showed MR. PI increased in all patients from 1.5 ± 0.45 at t0 to 2.4 ± 0.56 at t1, 2.6 ± 0.47 at t2, and 3.0 ± 0 at t3. The increase in PI between t0 and each individual timepoint from t1 to t3 showed statistical significance. Conclusions: The present results indicate the suitability and benefit of immediate provisionalization to achieve favorable peri-implant soft tissue conditions and papilla formation.
Implantologie, 1/2024
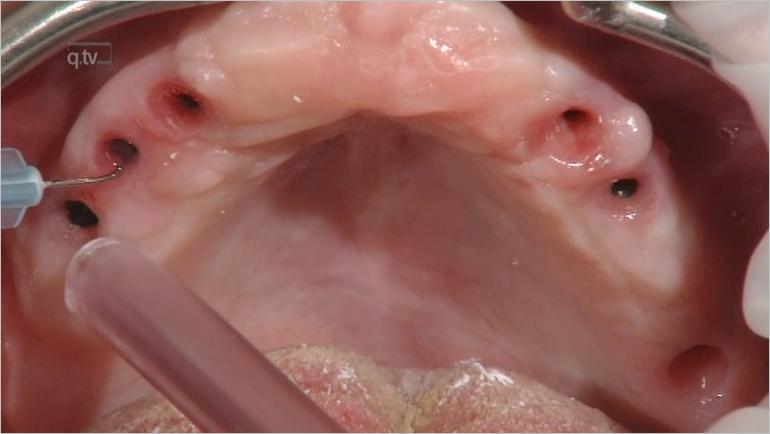
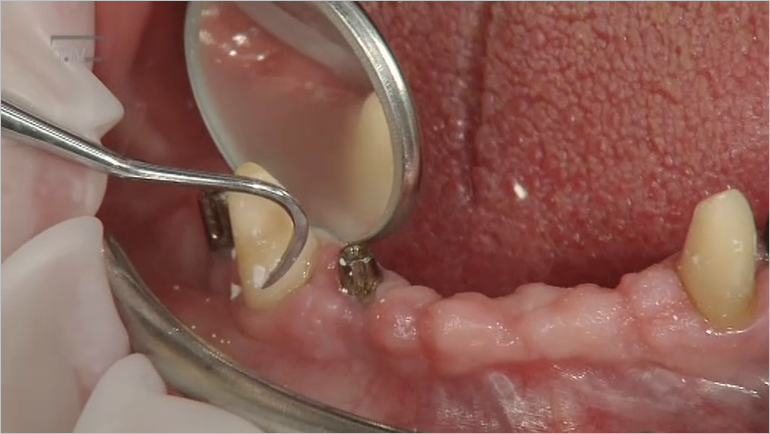
Seiten: 33-48, Sprache: DeutschLorenz, Jonas / Mitschikjan, Aram / Bornmann, Toni / Gerovac, Dragana / Weigl, Paul / Sader, RobertNotwendigkeit von Modifikationen des Behandlungsplans, technische Komplikationen sowie Hart- und WeichgewebeparameterDie Sofortversorgung im zahnlosen Kiefer bietet dank beschleunigter Behandlung und reduzierter Behandlungstermine viele Vorteile im Vergleich zur konventionellen Versorgung. Das Ziel der in diesem Beitrag vorgestellten klinischen Studie war die Untersuchung eines neuartigen Implantatsystems mit progressivem Gewindedesign für die Sofortversorgung des zahnlosen Kiefers auf vier Implantaten. Dabei wurden die Notwendigkeit von Modifikationen des Behandlungsplans, technische Komplikationen im Rahmen der Implantation und Sofortversorgung sowie Hart- und Weichgewebeparameter nach einjähriger Belastung dokumentiert. In die Studie eingeschlossen waren insgesamt zehn Studienteilnehmer, bei denen die Insertion von 40 Implantaten und deren sofortige provisorische Versorgung erfolgten. Während der provisorischen Phase kam es in einem Fall zu einem Verlust der provisorischen Versorgung einschließlich der vier Implantate. Zudem ging ein weiteres Implantat verloren. Die Guided-Surgery-Planungen bedurften keiner Modifikationen. Im Gegensatz dazu waren bei den Implantatinsertionen und den provisorischen Versorgungen Anpassungen erforderlich. Intraoperativ waren in den meisten Fällen kleinere Variationen des Behandlungsplans nötig, bis hin zur freihändigen Insertion von zwei Implantaten. Die klinischen und radiologischen Ergebnisse der Abschlussuntersuchung nach definitiver prothetischer Versorgung und einer mittleren Belastungsdauer von 16 Monaten (10−24 Monate) sprechen für gesunde periimplantäre Verhältnisse und eine hohe Patientenakzeptanz.
Schlagwörter: Sofortversorgung, zahnloser Kiefer, Guided Surgery, Implantaterfolg
International Journal of Periodontics & Restorative Dentistry, 5/2019
DOI: 10.11607/prd.4178, PubMed-ID: 31449586Seiten: 737-744, Sprache: EnglischNguyen, Vinh / von Krockow, Nadine / Pouchet, Joanne / Weigl, Paul MartinAlveolar ridge preservation procedures have been shown to significantly reduce the loss of ridge dimension of an extraction socket. As of yet, none of the alveolar ridge preservation techniques have been proven totally effective in preserving ridge morphology. The Periosteal Inhibition technique for alveolar ridge preservation involves placing a high-density polytetrafluoroethylene (d-PTFE) membrane between the periosteum and the buccal bone plate of an extraction socket. The authors hypothesize that the nonresorbable d-PTFE membrane, because of its much smaller pore diameter as compared to the size of the osteoclast precursor cells, inhibits the migration of the osteoclast precursor cells from the periosteum to the bony surface and, subsequently, their fusion to form osteoclasts. As a result, osteolytic activity on the outer surface of the socket is inhibited. The Periosteal Inhibition technique for alveolar ridge preservation is presented along with immediate implant treatment results using this treatment concept. The resulting stable ridge dimensions in these cases demonstrate a possibility that the d-PTFE membrane may effectively prevent modeling of the extraction socket by inhibiting the formation of osteoclasts on the outer bony surface.
Quintessence International, 4/2019
DOI: 10.3290/j.qi.a42160, PubMed-ID: 30887961Seiten: 278-285, Sprache: EnglischKroiss, Sebastian / Rathe, Florian / Sader, Robert / Weigl, Paul / Schlee, MarkusObjectives: The present preference clinical trial compared the long-term outcome of acellular dermal matrix allograft (ADMA) versus autogenous connective tissue graft (CTG) in the treatment of gingival recessions.
Method and materials: Thirty-nine consecutive patients with 233 Miller Class I and II recessions were treated by one operator (MS) with coronally advanced flaps and in addition either ADMA or CTG harvested from their palate. Clinical parameters were measured by an independent and masked assessor at baseline, 6 months, and 5 years.
Results: Thirty-two patients could be recruited for long-term examination (seven dropouts). At 6 months and 5 years, all clinical parameters showed significant improvements in both groups with slightly better but statistically not significant clinical results for CTGs. At 5 years, the CTG group revealed an additional gain of keratinized mucosa width (t6m-0: CTG 1.88 mm, ADMA 1.04 mm, P = .081; and t5y-0: CTG 3.98 mm, ADMA 3.06 mm, P = .01) compared to 6 months, whereas the mean for ADMAs remained stable (intergroup comparison statistically significant, P = .010). In all other parameters in both groups, slight but not statistically significant relapses were detected. Only one minor postoperative complication at one ADMA-treated site occurred.
Conclusions: Regarding the long-term results, ADMA could be an alternative treatment option to thicken soft tissue and to cover multiple gingival recessions. If the gain of keratinized mucosa width is considered as a main goal, CTG may have a slight advantage over ADMA.
Schlagwörter: acellular dermal matrix, connective tissue, gingival recession, long-term outcome, root coverage
The International Journal of Oral & Maxillofacial Implants, 1/2019
DOI: 10.11607/jomi.6717, PubMed-ID: 30695084Seiten: 25-30, Sprache: EnglischZhao, Liguo / Weigl, Paul / Wu, Yanyun / Xu, YuanzhiPurpose: To investigate the optimal degree of convergence of the abutment with which the bond strength achieved by the pre-bonding method is comparable with that in direct bonding with a conventional degree of convergence.
Materials and Methods: Abutments with 5.5-mm diameter, 5-mm height, 0.5-mm shoulder width, and three kinds of degrees of convergence (2, 4, and 6 degrees) were first designed by digital modeling. Their corresponding inner crowns were also modeled, and a gap of 40 μm was kept between the abutment and the inner crown. Thirty abutments and 30 inner crowns were then lathed out from a titanium plate (10 sets per degree of convergence). Six groups were defined in this study, according to the different degrees of convergence and bonding methods (direct bonding, pre-bonding) (n = 10 sets). The samples handled with direct bonding would be cleaned for reuse in tests with pre-bonding. Temporary cement was used as an adhesive, and the bond strength was tested in each set of samples. The comparison among the results was performed by the Kruskal-Wallis test.
Results: The mean values of bond strength with direct bonding methods were 349.39 ± 65.75 N, 316.49 ± 54.22 N, and 277.49 ± 56.96 N, and with pre-bonding methods were 279.35 ± 48.58 N, 227.97 ± 26.72 N, and 154.6 ± 23.03 N, respectively (2, 4, and 6 degrees). No statistical difference was found among the values in direct bonding groups and, in pre-bonding groups, only the comparison between 2 and 6 degrees of convergence showed statistical significance (P = .000). Between different bonding methods, statistical differences were shown in abutments with 4 and 6 degrees of convergence (P = .006, P = .000), respectively. The bond strength with pre-bonding methods and 2 degrees of convergence showed no significant difference from that with direct bonding and 6 degrees of convergence.
Conclusion: The bond strength was inversely proportional to the degree of convergence, and the bond strength of pre-bonding was lower than that of direct bonding with the same degree of convergence. When using the pre-bonding method, the bond strength between the abutment and inner crown with 2 degrees of convergence could be comparable with using the direct bonding method and abutments with conventional degrees of convergence.
Schlagwörter: bond strength, degrees of convergence, pre-bonding
Quintessenz Zahnmedizin, 6/2018
ImplantologieSeiten: 658-674, Sprache: DeutschTrimpou, Georgia / Parvini, Puria / Schwarz, Frank / Sader, Robert / Weigl, PaulTherapieregime für unterschiedliche ästhetische AusgangssituationenEine implantatverankerte Einzelkrone im ästhetisch sichtbaren Bereich, welche mit den benachbarten Strukturen nachhaltig perfekt harmoniert, ist bekanntlich eine große Herausforderung. Die Entscheidung für das Therapieregime einer Sofortimplantation und -versorgung bedingt daher eine sorgfältige Indikationsstellung mit entsprechender Beurteilung von Hart- und Weichgewebe des zu ersetzenden Zahnes und seiner Nachbarzähne. Indiziert das Resultat dieser Beurteilung ein Therapiekonzept zur Optimierung des ästhetischen Gesamtergebnisses, muss ein additives Gewebsmanagement erfolgen. Letzteres macht eine für den jeweiligen Patienten vorteilhafte Auswahl von chirurgischen und/oder kieferorthopädischen Maßnahmen sowie ggf. die Anwendung einer Zahnreplantation notwendig. Zusätzlich ist das Zeitregime der genannten adjuvanten Eingriffe in Relation zur Sofortimplantation und -versorgung zu definieren. Die daraus resultierende Komplexität soll mit Hilfe von in dem Beitrag vorgestellten Entscheidungsbäumen leichter handhabbar und so die Erstellung von fallspezifischen Therapieregimen erleichtert werden.
Schlagwörter: Sofortimplantation, Sofortversorgung, Frontzahntrauma, Frontzahnverlust, Zahnreplantation, kieferorthopädische Extrusion, Weichgewebsmanagement, Knochenaugmentation, Therapie-regime, Frontzahnästhetik, entzündliche Extraktionsalveole, Weichgewebsrezession
International Journal of Oral Implantology, 5/2016
SupplementPubMed-ID: 27314114Seiten: 89-106, Sprache: EnglischWeigl, Paul / Strangio, AntonioAim: The purpose of this literature review is to systematically evaluate the impact of immediate implant placement and restoration (IIPR) on hard and soft tissues and to identify clinical parameters which influence the outcome.
Materials and methods: An electronic search of the PubMed database was performed from January 2000 to September 2015. A further hand search was conducted in selected journals and only abstracts published in English were considered for review. Human clinical trials with at least 10 participants and which reported hard and soft tissue outcomes were assessed. Randomised controlled trials (RCT), prospective, prospective comparative and retrospective studies were considered. The effects of the following clinical parameters on hard and soft tissue outcomes were analysed: type of implant, primary stability, gingival biotype, flapless surgery, tooth extraction, spatial arrangement of the implant, socket grafting, the gap between implant surface and alveolar wall and the loading protocol.
Results: 17 studies (four RCT, six prospective, two comparative prospective, three controlled cohort and two retrospective studies) were included with 626 censored IIPR in 609 patients. A total of 411(65.56 %) implants were placed flapless vs 215 implants after raising a mucoperiosteal flap. Five studies defined raising a mucoperiostal flap as a mandatory part of the surgical protocol. The mean of the remaining gap in between the implant surface and the alveolar wall, the so-called "jump space", was reported for 170 implants ranging from 1.38 mm to 2.25 mm. Two hundred and one implant sites were not grafted, 405 were grafted, mostly with bone substitutes; for 20 no information was available. For 419 implants, a minimum insertion torque of ≥ 32 Ncm or an ISQ value of ≥ 60 was reached; for 53 implants an insertion torque of 25 Ncm was accepted. The implants were mostly placed palatinally of the jaw bone. The vertical position of the platform was reported either to be 0.5 to 1.0 mm below the vestibular bone crest or 3 to 4 mm apical to the adjacent cementoenamel junction of the neighbouring tooth. Post-insertion healing with a non-functional occlusion occurred for 97.8% of the implants. The final single crowns were inserted 3 to 6 months after implant placement. The IIPR resulted in a high success (97.96 %) and survival rate (98.25%) after a mean followup period of 31.2 months. The soft-tissue biotype was evaluated in 379 (60.5%) sites as thick. The mean crestal bone and the mean interproximal mucosa level changes were less than 1 mm compared to the baseline. The midfacial periimplant mucosal level change was less than 0.95 mm. This level was reached for both thin and thick soft-tissue biotypes, without a significant difference. Only in one study did the thin biotypes show a significantly higher recession.
Conclusion: The systematic review revealed promising results for immediately placed and immediately restored implants (IIPR) in the anterior maxilla. The possible options of flapless surgery and absence of grafting of the socket allows a minimal surgical intervention. However, a strict patient selection seemed mandatory for all included clinical trials.
Schlagwörter: immediate implant placement, immediate implant restoration, peri-implant tissue remodelling, single-tooth replacement