2019-1
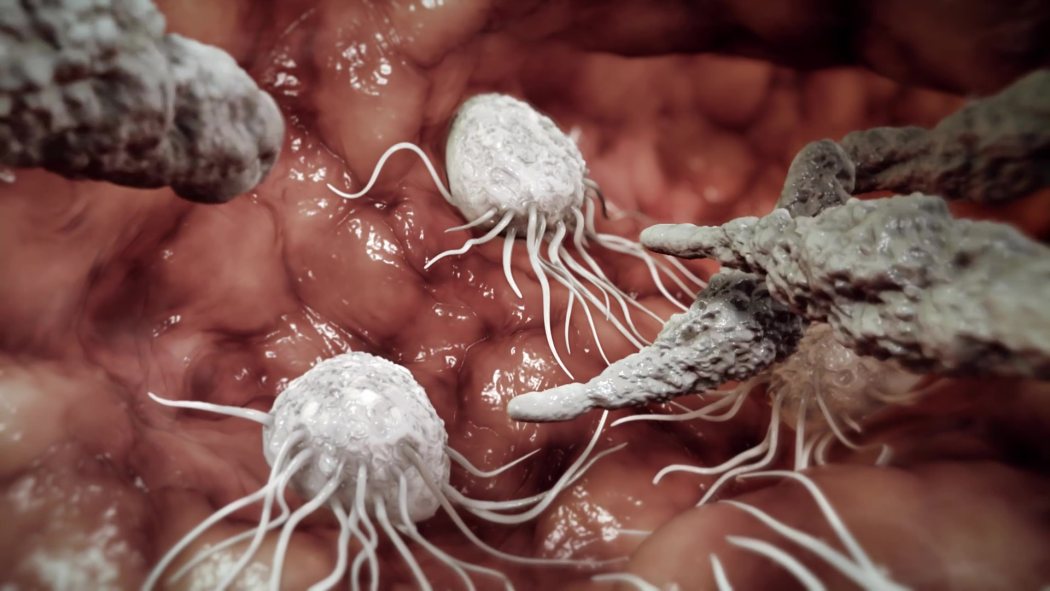
Seiten: 64-69, Sprache: EnglischStadlinger, Bernd / Jepsen, Søren / Terheyden, Hendrik / Heitz-Mayfield, Lisa J. A. / Berglundh, TordThis complementary article was prepared by Bernd Stadlinger, Søren Jepsen and Hendrik Terheyden and presents an overview of the content of the 6th volume of the "Cell-to-Cell Communication" series. The 6th volume of the series entitled "Peri-implantitis and its prevention" was prepared by a collaborative team of authors - Tord Berglundh, Søren Jepsen, Bernd Stadlinger, Hendrik Terheyden - and an advisory board. This computer-animated scientific film was launched at the EuroPerio meeting in Amsterdam in June 2018, providing a novel way to visualize the complex processes of peri-implant inflammation. It visualizes the biological background of the development and progression of peri-implantitis and highlights the importance of the microbiome and host immune defense. In addition, a perspective article has recently been published in the leading implant journal Clinical Oral Implants Research (Berglundh et. al. 2019). It is hoped that this complementary article will bring the film to the attention of the many ITI Fellows and Members who enjoy reading Forum Implantologicum. Please look for the Q reader at the end of the article and enjoy this captivating film.
The International Journal of Oral & Maxillofacial Implants, 7/2007
SupplementPubMed-ID: 18437797Seiten: 203-223, Sprache: EnglischQuirynen, Marc / Van Assche, Nele / Botticelli, Daniele / Berglundh, TordPurpose: To systematically review the current literature on the clinical outcomes and incidence of complications associated with immediate implants (implants placed into extraction sockets at the same surgery that the tooth is removed) and early implants (implants placed following soft tissue healing).
Materials and Methods: A Medline search was conducted for English papers on immediate/early placement of implants based on a series of search terms. Prospective as well as retrospective studies (randomized/nonrandomized clinical trials, cohort studies, case control studies, and case reports) were considered, as long as the follow-up period was at least 1 year of loading and at least 8 patients and/or at least 10 implants had been examined. Screening and data abstraction were performed independently by 3 reviewers. The types of complications assessed were implant loss; marginal bone loss; soft tissue complications, including peri-implantitis; and esthetics.
Results: The initial search provided 351 abstracts, of which 146 were selected for full-text analysis. Finally, 17 prospective and 17 retrospective studies were identified, with observation times generally between 1 and 2 years for the prospective studies and around 5 years for the retrospective studies. The heterogeneity of the studies (including postextraction defect characteristics, surgical technique with or without membrane and/or bone substitute, implant location in socket, inclusion and exclusion criteria, and prosthetic rehabilitation), however, rendered a meta-analysis impossible. Most papers contained only data on implant loss and did not provide useful information on failing implants or on hard and soft tissue changes. In general, the implant loss remained below 5% for both immediate and early placed implants (range, 0% to 40% for immediate implants and 0% to 9% for early placed implants), with a tendency toward higher losses when implants were also immediately loaded.
Conclusion: Because of the lack of long-term data, questions regarding whether peri-implant health, prosthesis stability, degree of bone loss, and esthetic outcome of immediate or early placed implants are comparable with implants placed in healed sites remain unanswered.
Schlagwörter: dental implants, early placement, extraction, immediate placement, osseointegration, partial edentulism, periodontology
Implantologie, 2/2005
SupplementSeiten: 139-148, Sprache: DeutschSchou, Søren / Berglundh, Tord / Lang, Niklaus P.Bei Periimplantitis mit ausgeprägter Taschenbildung (> 5 mm) und Knochenresorption können nach Abklingen der akuten Infektion und Einleiten einer korrekten Mundhygiene die verbliebenen Läsionen chirurgisch behandelt werden. Mittels Literaturrecherche wurde der aktuelle Kenntnisstand zu diesen Eingriffen im Bereich von handelsüblichen Reintitan-Implantaten ausgewertet. Tierversuche zu Implantaten mit rauer Oberfläche haben jüngst gezeigt, dass Osteoplastiken mit membrangedeckten autologen Knochenpartikeln zu einer beträchtlichen Geweberegeneration und Reosseointegration führen können. Diese experimentellen Studien sind aber nicht ohne weiteres auf den Menschen übertragbar, weil bei Tier und Mensch bisher unterschiedliche Implantattypen, Augmentationsmethoden, Analyseverfahren und Behandlungsmethoden (einschließlich Dekontamination der Implantatoberfläche) verwendet wurden. Fundierte Empfehlungen zur chirurgischen Behandlung von Periimplantitis können daher aus heutiger Sicht nicht gegeben werden. Hierzu wären weitere klinische Langzeitstudien mit genügend Teilnehmern erforderlich. Zudem waren die guten Resultate im Tierversuch auf Implantate mit sandgestrahlten/säuregeätzten Oberflächen beschränkt. Für Implantate mit anderen (insbesondere gedrehten) Oberflächen liegen keine entsprechenden Resultate vor. Im Zusammenhang mit der chirurgischen Behandlung von Periimplantitis wurden zahlreiche Methoden zur Dekontamination vorgeschlagen. Der einfachste und wirksamste Weg besteht vielleicht darin, dass man die titanplasmabeschichteten oder sandgestrahlten/ säuregeätzten Implantatoberflächen mit einem Gazestück behandelt, das abwechselnd mit Chlorhexidin und Kochsalzlösung getränkt wird.
Schlagwörter: Behandlung, Dentalimplantate, Pathologie, periimplantäre Infektionen, Periimplantitis
Implantologie, 2/2005
SupplementSeiten: 149-154, Sprache: DeutschLang, Niklaus P. / Berglundh, Tord / Heitz-Mayfield, Lisa J. / Pjetursson, Bjarni E. / Salvi, Giovanni E. / Sanz, MarianoThe International Journal of Oral & Maxillofacial Implants, 7/2004
SupplementSeiten: 140-149, Sprache: EnglischSchou, Søren / Berglundh, Tord / Lang, Niklaus P.Surgical treatment of peri-implantitis lesions can be performed in cases with considerable pocket formation (larger than 5 mm) and bone loss after the acute infection has been resolved and proper oral hygiene has been instituted. A literature review was conducted to ascertain current knowledge about surgical treatment options for peri-implantitis around commercially pure titanium implants. Recently reported animal studies involving implants with a rough surface indicate that considerable bone regeneration and re-osseointegration can be obtained by using membrane-covered autogenous bone graft particles. However, comparisons of the treatment outcomes in studies involving humans and animals are difficult because of differences in implant type, graft type, and evaluation protocols. In addition, different treatment procedures, including implant surface decontamination methods, have been used. Therefore, further long-term studies in humans involving sufficient numbers of subjects are needed to provide a solid basis for recommendations regarding the surgical treatment of peri-implantitis. Moreover, the encouraging treatment outcomes of regenerative procedures recently revealed in animal experiments and applied in the treatment of peri-implantitis around implants with sandblasted/acid-etched surfaces have not yet been documented for implants with other surfaces, especially turned surfaces. Numerous implant surface decontamination methods have been suggested as part of the surgical treatment of peri-implantitis. Decontamination of affected implants with titanium plasma-sprayed or sandblasted/acid-etched surfaces may most easily and effectively be achieved by applying gauze soaked alternately in chlorhexidine and saline.
The International Journal of Oral & Maxillofacial Implants, 7/2004
SupplementSeiten: 150-154, Sprache: EnglischLang, Niklaus P. / Berglundh, Tord / Mayfield, Lisa J. Heitz / Pjetursson, Bjarni E. / Salvi, Giovanni E. / Sanz, MarianoIntroductory remarks
The working group based its discussion on 2 systematic reviews published in 2002, 2 systematic reviews published in 2004 on related topics, and 3 traditional reviews prepared specifically for this consensus workshop (see reference list).
After extensive discussion, the previously unpublished reviews were amended where indicated, and consensus was reached that the reviews were both comprehensive and complete in covering the available published literature up to August of 2003. Hence, the papers were accepted and formed the basis for the consensus report on implant survival and complications. Subsequent to the consensus meeting, the quoted literature was updated up to December 2003.
For the purpose of clarification and understanding of the evaluated literature, the working group adopted a glossary of terms.
The International Journal of Oral & Maxillofacial Implants, 3/2001
Seiten: 323-332, Sprache: EnglischAbrahamsson, ngemar / Zitzmann, Nicola U. / Berglundh, Tord / Wennerberg, Ann / Lindhe, JanThe aim of the present experiment was to study the peri-implant soft and hard tissues formed at titanium implants with 2 different surface configurations and to give a topographic description of the surfaces examined. In 5 beagle dogs, the mandibular premolars were extracted. Three months later, 4 self-tapping standard implants (SI) and 4 Osseotite implants (OI) of the 3i Implant System were placed. The marginal 3 mm of the OI is turned, while the remaining part has an acid-etched surface structure. Abutments were connected after 3 months. A plaque control period was initiated, and after 6 months block biopsies were obtained. From each animal 2 units of each implant type were processed and embedded in EPON. The remaining biopsies were processed for ground sectioning. The histometric measurements performed on the EPON sections revealed that the peri-implant soft tissues and the marginal level of bone-to-implant contact were similar for SI and OI sites. In the ground sections, bone-to-implant contact (BIC%) and bone density assessments were made in 2 different zones. Zone I represented the contact area measured from the marginal level of bone-to-implant contact (B) to a position 4 mm above the apex of the implant, and zone II represented the apical 4 mm of the implant. For the SI sites, the BIC% was 56.1% in zone II and 58.1% in zones I + II. The corresponding figures for the OI sites were 76.7% and 72.0%. The BIC% was significantly larger at OI than at SI sites. Bone density values were similar at the SI and OI sites.
International Journal of Periodontics & Restorative Dentistry, 3/2001
Seiten: 289-295, Sprache: EnglischZitzmann, Nicola U. / Schärer, Peter / Marinello, Carlo P. / Schüpbach, Peter / Berglundh, TordThe aim of the present study was to investigate the healing of alveolar ridge defects augmented with cancellous bovine bone mineral. In six partially edentulous patients, bone augmentation was necessary prior to implant placement because of severe alveolar ridge resorption. The defect sites, all located in the maxilla, were filled with Bio-Oss and covered with the resorbable collagen membrane Bio-Gide. Biopsies were obtained from the defect sites 6 to 7 months following grafting and were processed for ground sectioning. The histologic analysis revealed that the Bio-Oss particles occupied 31% of the total biopsy area. An intimate contact between woven bone and Bio-Oss was detected along 37% of the particle surfaces. A mixed type of bone was found; it contained woven bone and parallel-fibered bone, which demonstrates features of remodeling activity. Signs of resorption of the grafting material were observed in the histologic sections, which indicates that the material takes part in the remodeling process. It is suggested that Bio-Oss may be a very suitable material for staged localized ridge augmentation in humans.