Implantologie, 1/2025
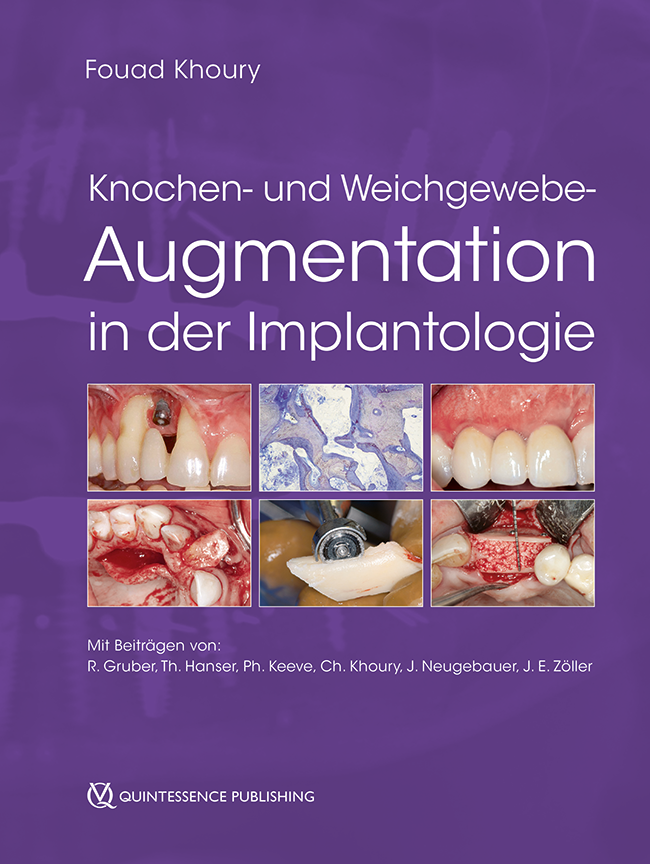
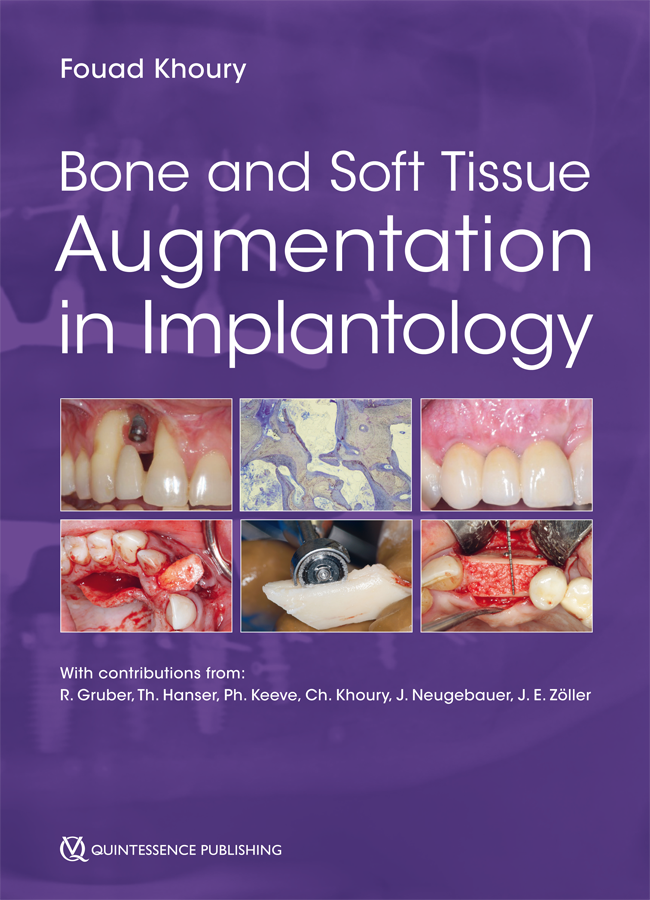
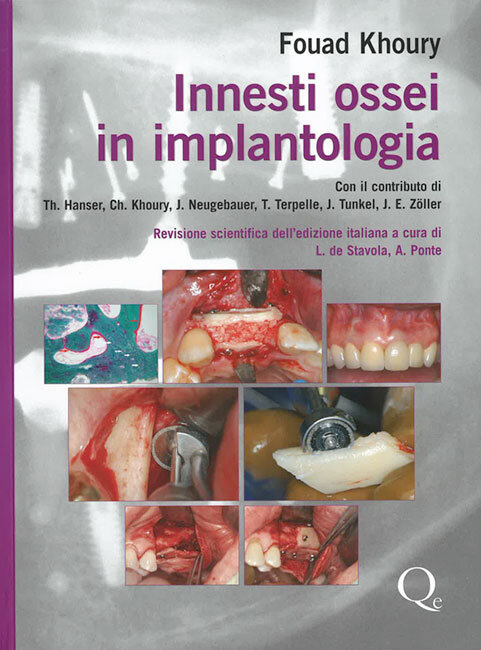
Seiten: 23-35, Sprache: DeutschKhoury, Elias Jean-Jacques / Hampe, Tristan / Khoury, FouadAugmentative Verfahren zeigen hohe Erfolgsraten, jedoch bleiben peri- und postoperative Komplikationen ein wichtiges Thema in der Praxis. Eine sorgfältige präoperative Bewertung individueller Risikofaktoren wie Rauchen, Diabetes oder systemische Medikation ist entscheidend, um die Heilung und langfristige Stabilität zu fördern. Zu den häufigsten Herausforderungen zählen die Exposition des Knochenmaterials nach Augmentation und das Risiko einer Sinusinfektion nach Sinusbodenelevation. Präventive Maßnahmen wie spezifische Schnitttechniken, optimale Weichgewebedeckungen, gezielte Antibiotikaprophylaxe und operative Protokolle unter Berücksichtigung biologischer Prinzipien unterstützen den erfolgreichen Heilungsverlauf und reduzieren das Risiko für Komplikationen.
Schlagwörter: Knochenaugmentation, Knochenentnahme, Komplikationen, Schalentechnik, Knochenexposition, Weichteilnekrosen, Wunddehizenz, MicroSaw, Sinusbodenelevation
International Poster Journal of Dentistry and Oral Medicine, 1/2025
Poster 2684, Sprache: Englisch, DeutschPolly, Christoph / Hampe, Tristan / Khoury, FouadEinleitung: Bei einer engen anatomischen Lagebeziehung von verlagerten Zähnen zum Nervus alveolaris inferior birgt die operative Entfernung eine erhöhte Gefahr der Nervschädigung. Eine Koronektomie, bei der die Wurzel im Kiefer verbleibt, kann dieses Risiko verringern. Das angeführte Fallbeispiel zeigt eine Koronektomie mit nachfolgender implantologischer Rehabilitiation. Material und Methoden: Die Patientin stellte sich mit einem distalangulierten verlagerten Zahn 45 sowie Sekundärkaries an dem mesialen Kronenrand von Zahn 47 vor. Die Zähne 45 und 46 waren seit Jahrzehnten durch Brückenglieder ersetzt, wobei 44 und 47 als Brückenpfeiler dienten. 3D-Bildgebung zeigte, dass der Nervus alveolaris inferior von der Wurzel des Zahns 45 umschlossen war. Eine Koronektomie an Zahn 45 wurde empfohlen und unter intravenöser Sedierung mit perioperativer antibiotischer Abschirmung durchgeführt. Für den Zugang wurde mit der MicroSaw ein Knochendeckel angelegt. Die Zahnkrone und das koronale Drittel der Wurzel wurden entfernt, und die verbleibende Wurzel wurde aufgrund ihrer Nähe zum Nerv belassen. Anschließend wurde der Knochendeckel reponiert. Nach einer komplikationslosen Wundheilung wurde der Zahns 47 nach dem Scheitern eines Erhaltungsversuchs entfernt. Zwei Monate postoperativ erfolgte die Implantation in regio 45 und 47 und die Knochenaugmentation mittels Split-Bone-Block- und „Carota“-Technik. Autologer Knochen wurde lokal und aus dem ipsilateralen Retromolarbereich entnommen. Nach der Implantatfreilegung erfolgte die prothetische Versorgung ohne jegliche Sensibilitätseinschränkung im Versorgungsbereich des N. alveolaris inferior. Schlussfolgerung: Eine Koronektomie kann eine Alternative zur vollständigen Zahnentfernung darstellen, wenn eine enge Beziehung zum Nervus alveolaris inferior besteht. Die Anwendung der Knochendeckelmethode erhält den umgebenden Knochen und ermöglicht eine anschließende Implantation.
Schlagwörter: Koronektomie, Fallbericht, Schalentechnik, Autologer Knochen, Knochendeckel
International Journal of Oral Implantology, 1/2025
PubMed-ID: 40047363Seiten: 59-68, Sprache: EnglischHampe, Tristan / Khoury, FouadPurpose: Dislocation of implants into the maxillary sinus typically occurs during surgery or in the early postoperative period. This case study presents an instance of implant dislocation that occurred after 30 years under functional loading due to peri-implantitis. Materials and methods: An 87-year-old woman presented with a loosened fixed partial denture, revealing a missing implant in the maxillary left second molar site upon clinical examination. The patient showed no symptoms of sinusitis. Imaging confirmed the dislocation of the implant, along with a pathological radiodensity filling the sinus. Maxillary sinus revision was performed via a bone lid under conscious sedation. The implant was removed along with a polypous mass, and the latter was sent for pathological examination. Following debridement, disinfection (3% hydrogen peroxide, photodynamic decontamination) was performed. The oroantral fistula was closed through double-layer closure with a pedicled connective tissue flap and a mucoperiosteal flap. Two months after surgery, sinus floor elevation using the layering technique and implant placement were performed. After 3 months, the implants were exposed, and the restoration was placed 6 weeks later. Results: Histopathological examination confirmed chronic sinusitis with the presence of polyps. A 2-month follow-up CBCT scan revealed a healthy sinus with an open ostium. Subsequent procedures went uneventfully. Conclusions: Progressive peri-implantitis in the posterior maxilla can lead to the dislocation of dental implants into the sinus and subsequent chronic sinusitis. Removing the implant through a bone lid from the lateral sinus wall with simultaneous sinus revision is an effective way to treat this condition and allows for later bone grafting and implant placement.
Schlagwörter: bone lid, chronic sinusitis, dental implant dislocation, maxillary sinus, peri-implantitis
The authors declare there are no conflicts of interest relating to this study.
International Journal of Oral Implantology, 2/2022
PubMed-ID: 35546722Seiten: 111-126, Sprache: EnglischKhoury, Fouad / Hanser, ThomasPurpose: To evaluate the short- and long-term outcomes of vertical 3D bone augmentation in the posterior mandible, performed using the split bone block technique with a tunnel technique.
Materials and methods: Patients were treated for vertical and horizontal alveolar bone defects without simultaneous implant placement and followed up for at least 10 years postoperatively. Autogenous bone blocks were harvested from the mandibular retromolar area following the MicroSaw protocol (Dentsply Sirona, Charlotte, NC, USA). The harvested bone blocks were split longitudinally according to the split bone block technique and grafted in 3D form using a tunnel technique. Implants were inserted and exposed after 3 months and prosthetic restoration was performed.
Results: A total of 117 consecutively treated patients with 128 grafted sites in 3D form were enrolled in the present study and followed up over a period of up to 17 years. The 10-year results were collected with a total patient dropout rate of 24.13%. Minimal late graft exposure was documented postoperatively for 4 to 8 weeks on the lingual site in two cases but did not influence the outcome. Infection of the grafted area occurred in one other case, leading to loss of the grafted bone. The postoperative mean vertical bone gain was 7.6 ± 3.1 mm and the mean bone width achieved after surgery was 8.1 ± 1.6 mm. A total of 287 implants were inserted 3 months after the augmentation procedure. The maximum vertical bone resorption, which was calculated around implants, was 0.66 ± 0.38 mm after 1 year, 0.72 ± 0.31 mm after 5 years and 0.75 ± 0.43 mm after 10 years. Furthermore, five implants were lost during this time, due to peri-implantitis and chronic pain. After 10 years, the mean vertical bone gain was stable at 6.72 ± 2.26 mm and the resorption rate was 11.4%.
Conclusions: The short- and long-term results of the present study confirm the predictability of using mandibular bone blocks according to the split bone block technique for 3D bone reconstruction in the posterior mandible.
Schlagwörter: 3D bone augmentation, MicroSaw protocol, posterior mandible, split bone block technique, tunnel technique, vertical alveolar crest augmentation
Conflict-of-interest statement: This study was completely self-supported and no contribution from any commercial party was received, even in the form of free materials.
Implantologie, 2/2022
Seiten: 193-202, Sprache: DeutschKhoury, Fouad / Zastera, AlexanderErfahrungsbericht und technische HinweiseDie Rekonstruktion von Kieferkammdefekten mit autologen Knochentransplantaten stellt in der dentalen Implantologie den Goldstandard dar. Durch eine schonende Implantatbettaufbereitung und gleichzeitige minimalinvasive Knochenentnahme mittels Trepanbohrung aus dem zukünftigen Implantatbett können lokal gewonnene autologe Knochenkerne zur Rekonstruktion von knöchernen Kieferkammdefekten simultan zur Implantatinsertion genutzt werden. Die Karottentechnik zeichnet sich als autologe Augmentationstechnik durch hohe osteogenetische, osteokonduktive und osteoinduktive Potenziale aus. Vorteile bieten, neben der Reduzierung der Behandlungszeit, die geringere Morbidität durch den Entfall einer zusätzlichen Entnahmestelle und der Verzicht auf Membranen oder Ersatzmaterialien anderer Herkunft.
Manuskripteingang: 22.02.2022, Annahme: 05.05.2022
Schlagwörter: Karottentechnik, minimalinvasive Augmentation, Knochentransplantation, Knochenkerntechnik, zweiteiliger Trepanbohrer, Microscrew, Implantate
The International Journal of Oral & Maxillofacial Implants, 2/2019
DOI: 10.11607/jomi.6869, PubMed-ID: 30883623Seiten: 471-480, Sprache: EnglischKhoury, Fouad / Hanser, ThomasPurpose: The aim of this clinical study was to evaluate the long-term outcome of the split bone block (SBB) technique for vertical bone augmentation in the posterior maxilla in combination with sinus floor elevation using a tunneling approach.
Materials and Methods: Patients were treated for extensive vertical and horizontal alveolar bone defects without simultaneous implant placement and followed up for at least 10 years postoperatively. Autogenous bone blocks were harvested from the mandibular retromolar area following the MicroSaw protocol. The harvested bone blocks were split longitudinally according to the SBB technique. Implants were inserted and exposed after every 3 months, and prosthetic restoration was performed.
Results: One hundred forty-two consecutively treated patients, 154 grafted sites, and 356 inserted implants were documented. Minimal graft exposure (1 to 3 mm) 4 to 8 weeks postoperatively was documented in two sites; infection of the grafted area occurred in one other case. The mean preoperative clinical vertical defect was 7.8 ± 3.9 mm, and the mean horizontal width was 3.1 ± 2.2 mm. Postoperatively, the mean vertical gained dimension was 7.6 ± 3.4 mm (maximum: 13 mm), and the mean width was 8.3 ± 1.8 mm. Implants could be inserted in all sites, with additional local small augmentation in 21 cases. The amount of maximum vertical bone resorption was 0.21 ± 0.18 mm after 1 year, 0.26 ± 0.21 mm after 3 years, 0.32 ± 0.19 mm after 5 years, and 0.63 ± 0.32 mm after 10 years. As part of a total patient dropout of 16.9%, four implants were lost within 10 years. The mean vertically gained bone was stable at 6.82 ± 0.28 mm (maximum: 12 mm). The resorption rate after 10 years was 8.3%.
Conclusion: The described tunneling flap approach allows a hermetic soft tissue closure, characterized by a reduction of dehiscence and a secure bone graft healing. The combination of thin autogenous bone blocks and bone particles according to the SBB technique allows an acceleration of transplant revascularization, and thus, of graft regeneration, allowing a shortening of the patient treatment time as well as long-term three-dimensional volumetric bone stability.
Schlagwörter: 3D bone augmentation, MicroSaw protocol, posterior maxilla, sinus floor elevation, split bone block technique, tunnel technique, vertical alveolar ridge augmentation
The International Journal of Oral & Maxillofacial Implants, 5/2018
DOI: 10.11607/jomi.6517, PubMed-ID: 30231102Seiten: 1136-1139, Sprache: EnglischKhoury, Fouad / Javed, Fawad / Romanos, Georgios E.Purpose: This observational study was based on a series of clinical cases in which failure of sinus augmentations occurred in patients who received prophylactic clindamycin therapy.
Materials and Methods: Between the years 2006 and 2010, a retrospective observational study was performed. The study consisted of 1,874 patients (723 males and 1,151 females) in whom sinus augmentations were performed prior to placement of dental implants.
Results: In nine (0.48%) patients (four males and five females), infection of the graft material inside the sinus floor occurred, and six patients developed an abscess in the site of surgery, 4 to 6 weeks postoperatively. In three patients, a buccal fistula with pus draining was observed 5 to 8 weeks postoperatively. In all patients, the source of infection was from the grafted material within the sinus. A common manifestation in all nine patients was that they had self-reported penicillin allergy and had been prescribed clindamycin (300 mg every 6 hours for 10 days).
Conclusion: Prophylactic clindamycin therapy following sinus augmentation procedures seems to be a risk factor for infections and loss of grafting material following these surgical techniques.
Schlagwörter: allergy, amoxicillin, clindamycin, infection, penicillin, resistance, sinus augmentation
International Journal of Periodontics & Restorative Dentistry, 2/2018
DOI: 10.11607/prd.3467, PubMed-ID: 29447312Seiten: 199-207, Sprache: EnglischKhoury, Fouad / Doliveux, RomainThe aim of this study was to evaluate a new minimally invasive surgical technique for the reconstruction of critical-size bony defect with local harvested bone core with simultaneous implant placement. In a prospective study, 186 consecutively treated patients were included and controlled clinically and radiologically for at least 5 years postoperative. Every patient presented a bony defect affecting the buccal, lingual, or palatal wall. In all cases, the alveolar crest was wide enough to allow implant placement inside the bony contours. During implant bed preparation, a trephine bur (3.5 mm external diameter and 2.5 mm internal diameter) was used to harvest a bone core from the socket. After implant insertion, the buccal/palatal/lingual bony defect was grafted with bone chips covered with the bone core stabilized through compression with microscrews. After 3 months of healing, the implants and the grafted bone were exposed and the width of the grafted area was measured. After prosthetic restoration, the patients were recalled regularly. A total of 223 grafted sites were documented. Minor primary healing complications were observed in 3 sites (1.4%), all in smoker patients, and were treated locally without any influence on the prognosis. All other sites healed uneventfully. In 19 cases (4.4%), exposure of the screw heads was detected 1 to 3 months postoperatively without any inflammation or consequences for the grafted bone. The average width of the reconstructed area at the end of the grafting procedure was 2.4 ± 0.8 mm, and at the reentry, 2.1 ± 0.6 mm. There was a difference of remodeling between bone cores grafted totally inside or partially outside the bony contours. Bone cores grafted completely inside the bony contours demonstrated no resorption at 3 months postoperative, while bone cores grafted partially outside the bony contours in most cases showed partial resorption of the bone outside the bony contours. After 3 months of healing, all 223 implants had achieved primary healing and osseointegration and were restored after an average time of 4 months. No implant failed during the control period. According to this study, the use of an autogenous bone core harvested during the implant bed preparation is a simple and safe method for the reconstruction of small bone defects.
The International Journal of Oral & Maxillofacial Implants, 5/2017
DOI: 10.11607/jomi.5832, PubMed-ID: 28906506Seiten: 1086-1096, Sprache: EnglischKhoury, Fouad / Keller, Pierre / Keeve, Philip L.Purpose: To evaluate long-term survival rates and radiographic stability of sinus floor elevations carried out using a two-layer grafting technique.
Materials and Methods: Records were analyzed for patients treated with sinus floor elevations using a modified technique. Phycogenic hydroxyapatite (Algipore, Dentsply Sirona Implants) and autogenous bone particles harvested from intraoral sites were grafted in two distinct layers after elevation of the sinus mucosae. In this approach, the basal part of the sinus floor is grafted with autogenous bone, while the cranial part is grafted with the phycogenic hydroxyapatite. In some cases, implants were placed simultaneously, such that the entire surface of each implant was covered by autogenous bone particles. A titanium membrane was used to close the sinus window, and the implants were loaded 3 months later. In two-stage approaches, the implants were inserted 3 to 4 months after the grafting and loaded after 3 additional months. Panoramic radiographs were taken after the grafting procedure, after implant insertion, after the prosthetic restoration, and then annually for 10 years. These radiographs were used to measure the height between the implant shoulders and the top of the graft.
Results: Of the 214 sinus floor elevations performed on 129 patients using the bilayering technique, 198 procedures in 118 patients were included in the study (136 one-stage and 62 two-stage). Membrane perforations during surgery occurred in 17.9% of the procedures and were sutured and sealed with fibrin glue. A total of 487 implants were placed in the grafted areas. No severe postoperative complications occurred, but three implants were lost throughout the 10-year follow-up period. A small decrease of vertical height was observed between the grafting surgery and the stage-two surgery (mean: 1.8 mm). After that, no bone height was lost over the 10 years.
Conclusion: The layer grafting technique in combination with sinus floor elevation resulted in radiographically stable vertical bone height for 10 years. This technique enabled early placement and loading of implants in the grafted areas. The survival rate obtained with this procedure is similar to that expected for implants placed in nongrafted areas.
Schlagwörter: Algipore, autogenous bone, bilayer technique, biomaterial, bone augmentation, graft stability, sinus floor elevation
The International Journal of Oral & Maxillofacial Implants, 1/2017
DOI: 10.11607/jomi.4880, PubMed-ID: 28095518Seiten: 137-146, Sprache: EnglischKeeve, Philip L. / Khoury, FouadPurpose: The aim of this retrospective study was to compare long-term (≥ 5 years) outcomes of implants placed in patients treated for chronic periodontitis versus those placed in periodontally healthy patients. In both groups, the implants were placed in alveolar ridges that were laterally augmented with autogenous bone block grafts using a split bone block technique.
Materials and Methods: Two hundred ninety-two patients were screened in the course of supportive periodontal treatment examinations. Nonsmoking patients without any severe systemic diseases who had adhered to regular supportive periodontal treatment for a minimum of 5 years after undergoing autogenous lateral grafting (using the split bone block technique), implant placement, and prosthetic reconstructions were classified into two groups based on their presurgical status: periodontally healthy patients (PHP) and periodontally compromised patients (PCP).
Results: Clinical outcomes for 77 patients, 38 PHP and 39 PCP, were examined. All had been successfully treated for severe lateral atrophy and received a total of 241 endosseous implants between 2002 and 2008. At the final examination, mean bleeding on probing was 7.08% ± 7.27% in PHP and 14.49% ± 18.14% in PCP, a statistically significant difference. Significantly higher Plaque Index and more recession were associated with a narrow ( 2 mm) width of keratinized mucosa.
Conclusion: Implants in alveolar ridges laterally augmented using a split bone block technique revealed similar clinical peri-implant conditions in both PHP and PCP. Using autogenous bone block grafts without biomaterials resulted in long-term peri-implant tissue stability.
Schlagwörter: autogenous bone augmentation, CIST, lateral augmentation, peri-implant disease, periodontally compromised patients, split bone block grafting