Quintessenz Zahnmedizin, 7/2025
EditorialSeiten: 595, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 7/2025
ZahnerhaltungSeiten: 609, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 6/2025
EditorialSeiten: 479, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 5/2025
Seiten: 401, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 4/2025
EditorialSeiten: 295-296, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 4/2025
ZahnerhaltungSeiten: 311-313, Sprache: DeutschFrankenberger, RolandDeutsche Zahnärztliche Zeitschrift, 4/2025
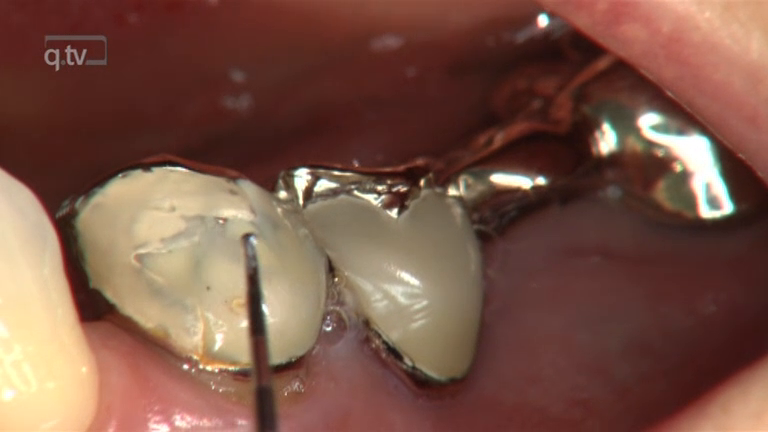
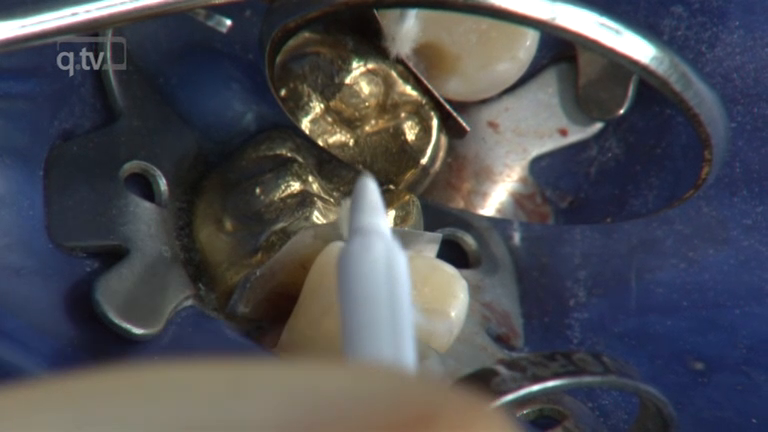
WissenschaftSeiten: 252-260, Sprache: DeutschFrankenberger, Roland / Friedrich, Katharina / Dudek, Marie-Christine / Winter, Julia / Krämer, Norbert / Roggendorf, Matthias J.Ziel: Das Vorhaben dieser In-vitro-Studie war es, den Einfluss approximal-zervikal unterminierter Schmelzränder auf die adhäsive Gesamtperformance (Randqualität und Schmelzintegrität/Rissbildung) unterschiedlich hergestellter (Labor vs. CAD/CAM) und unterschiedlich befestigter (Multistep-Adhäsiv vs. Universaladhäsiv) Keramikinlays und Keramikteilkronen zu untersuchen. Material und Methode: 192 extrahierte Weisheitszähne erhielten zirkulär schmelzbegrenzte mod-Präparationen für Keramikinlays (n = 96) und -teilkronen (n = 96). Der distale approximale Kasten diente als Kontrolle, im mesialen Kasten wurde im Dentin eine zervikale Rille von 2×2×4 mm angelegt, um eine dort tiefere (Dentin-)Kariesexkavation zu simulieren. Diese Dentinrille wurde entweder belassen (R/Rille), mit Komposit gefüllt (F/Füllung) oder komplett entfernt, wobei dann der zervikale Rand im Dentin/Zement zu liegen kam (D/Dentin). Laborgefertigte (e.max Press) und CAD/CAM-gefertigte (e.max CAD) mod-Inlays und Teilkronen wurden mit Syntac/Variolink Esthetic (SV) oder Adhese Universal/Variolink Esthetic (AV) adhäsiv befestigt. Bei den laborgefertigten Restaurationen wurde die Provisorientragezeit (1.000 Belastungszyklen und 25 Thermozyklen) ebenfalls simuliert. Initial (21 Tage Wasserlagerung) und erneut nach thermomechanischer Belastung (TMB: 1 Mio. Zyklen mit 50 N, 25.000 Thermozyklen mit 5 °C/55 °C) erfolgte die Herstellung von Epoxidharz-Replikas, die rasterelektronenoptisch (200-fache Vergrößerung) auf Randspalten untersucht wurden. An den Originalproben erfolgte lichtmikroskopisch (zehnfache Vergrößerung) die Evaluation der Risszunahme im approximal-zervikalen Bereich bei Labside-Restaurationen vor der provisorischen Versorgung und nach TMB, bei Chairside-Restaurationen vor und nach TMB. Ergebnisse: Unabhängig vom Adhäsivsystem zeigten generell die D-Gruppen eine signifikant schlechtere Randqualität (p 0,05), wobei das Universaladhäsiv besser performte als das Mehrschrittadhäsivsystem (p 0,05). Die Subgruppen R und F waren unabhängig vom Adhäsivsystem hinsichtlich der Randqualität zwar ähnlich (p > 0,05) und nicht schlechter als die Kontrollen (p > 0,05), zeigten aber bei F weniger Rissbildung als bei R (p 0,05). Bei CAD/CAM-Restaurationen wurden generell weniger Risse als bei laborgefertigten Restaurationen beobachtet (p 0,05). Teilkronen zeigten bessere Randqualitäten und weniger Risse als Inlays (p 0,05). Schlussfolgerungen: Liegt bei Keramikpräparationen nach der Kariesexkavation im approximalen Kasten das Dentinniveau tiefer als das Schmelzniveau, sollte die resultierende unterminierte Schmelzlamelle nicht entfernt werden. Stattdessen sollte der unterminierte Schmelz erhalten und der fehlende Dentinbereich mit einer adhäsiven Aufbaufüllung ausgeglichen werden. Bezüglich der Leistungsfähigkeit der untersuchten Adhäsive hat das Universaladhäsiv Adhese Universal den ehemaligen Goldstandard Syntac abgelöst.
Schlagwörter: Adhäsiv, etch-and-rinse, Inlay, Keramik, Randqualität, Rissbildung, self-etch, Teilkrone
Quintessenz Zahnmedizin, 3/2025
EditorialSeiten: 203, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 2/2025
EditorialSeiten: 103, Sprache: DeutschFrankenberger, RolandThe Journal of Adhesive Dentistry, 1/2025
Open Access Online OnlyCLINICAL MEDICINEDOI: 10.3290/j.jad.c_198030. Apr. 2025,Seiten: 75-80, Sprache: EnglischKrempels, Jacqueline Victoria / Sturm, Richard / Neumann, Konrad / Schumacher, Tamara / Schouten, Christian / Faber, Franz-Josef / Frankenberger, Roland / Roggendorf, Matthias JohannesPurpose: To investigate the effect of tooth age on dentin adhesion of different luting systems to the root canal.
Materials and Methods: 180 root canals of extracted teeth were divided into three age-specific groups (n = 60): young 20–35 (y), middle-aged 45–60 (m), and older 70–85 (o) years. Ten teeth of each age group were assigned to a luting system: Panavia 21 with ED Primer (P21, Kuraray); Core X Flow with Prime&Bond active and Self-Cure Activator (CXF, Dentsply Sirona); Multilink Automix with Multilink Primer (ML, Ivoclar Vivadent); Panavia SA Cement Plus (PSA, Kuraray); Smart Cem 2 (SM2, Dentsply Sirona); Speed CEM Plus (SCP, Ivoclar Vivadent).
The root canals of decoronated teeth were instrumented with F360 (Komet) and BR7 (FKG) up to a working length of 8 mm (Ø0.6mm, taper 0.02) and filled with standardized steel spreaders and the selected material. The intracanal bond was determined by a pull-out test. The failure modes were categorized as an adhesive to dentin (AD), adhesive to spreader (AS), cohesive within the composite (C), and mixed (M). Statistical analysis was performed using non-parametric ANOVA, Tukey, and Chi-square test at a significance level of α ≤ 0.05.
Results: The study showed significant differences for the various luting systems (ANOVA, P 0.05). PSA showed significant differences in bond strength to SM2, CXF, SCP, and ML, as did SM2 to P21 and SCP (Tukey, P 0.05). M (46%) occurred 53% in y and 70% in SCP.
Conclusions: No adhesive strategy can yet be recommended for tooth age. Clinically available luting systems show significant differences in their adhesion values.
Schlagwörter: luting systems, post adhesion, root canal dentin, tooth age