Quintessenz Zahnmedizin, 7/2025
EditorialSeiten: 595, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 7/2025
ZahnerhaltungSeiten: 609, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 6/2025
EditorialSeiten: 479, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 5/2025
Seiten: 401, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 4/2025
EditorialSeiten: 295-296, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 4/2025
ZahnerhaltungSeiten: 311-313, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 3/2025
EditorialSeiten: 203, Sprache: DeutschFrankenberger, RolandQuintessenz Zahnmedizin, 2/2025
EditorialSeiten: 103, Sprache: DeutschFrankenberger, RolandThe Journal of Adhesive Dentistry, 1/2025
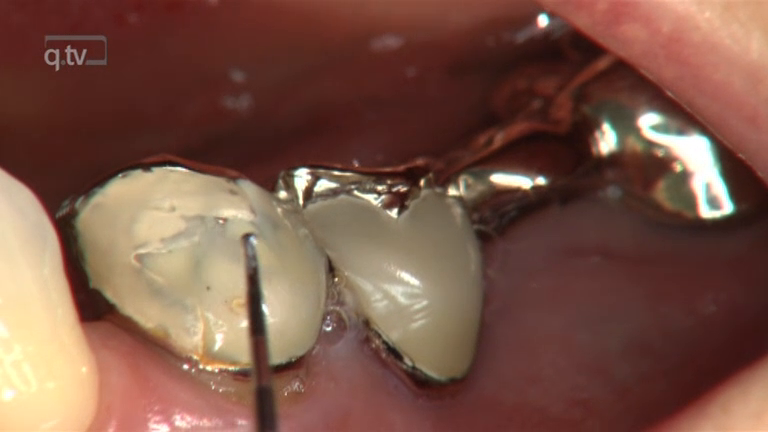
Open Access Online OnlyCLINICAL MEDICINEDOI: 10.3290/j.jad.c_1980April 30, 2025,Seiten: 75-80, Sprache: EnglischKrempels, Jacqueline Victoria / Sturm, Richard / Neumann, Konrad / Schumacher, Tamara / Schouten, Christian / Faber, Franz-Josef / Frankenberger, Roland / Roggendorf, Matthias JohannesPurpose: To investigate the effect of tooth age on dentin adhesion of different luting systems to the root canal.
Materials and Methods: 180 root canals of extracted teeth were divided into three age-specific groups (n = 60): young 20–35 (y), middle-aged 45–60 (m), and older 70–85 (o) years. Ten teeth of each age group were assigned to a luting system: Panavia 21 with ED Primer (P21, Kuraray); Core X Flow with Prime&Bond active and Self-Cure Activator (CXF, Dentsply Sirona); Multilink Automix with Multilink Primer (ML, Ivoclar Vivadent); Panavia SA Cement Plus (PSA, Kuraray); Smart Cem 2 (SM2, Dentsply Sirona); Speed CEM Plus (SCP, Ivoclar Vivadent).
The root canals of decoronated teeth were instrumented with F360 (Komet) and BR7 (FKG) up to a working length of 8 mm (Ø0.6mm, taper 0.02) and filled with standardized steel spreaders and the selected material. The intracanal bond was determined by a pull-out test. The failure modes were categorized as an adhesive to dentin (AD), adhesive to spreader (AS), cohesive within the composite (C), and mixed (M). Statistical analysis was performed using non-parametric ANOVA, Tukey, and Chi-square test at a significance level of α ≤ 0.05.
Results: The study showed significant differences for the various luting systems (ANOVA, P 0.05). PSA showed significant differences in bond strength to SM2, CXF, SCP, and ML, as did SM2 to P21 and SCP (Tukey, P 0.05). M (46%) occurred 53% in y and 70% in SCP.
Conclusions: No adhesive strategy can yet be recommended for tooth age. Clinically available luting systems show significant differences in their adhesion values.
Schlagwörter: luting systems, post adhesion, root canal dentin, tooth age
The Journal of Adhesive Dentistry, 1/2025
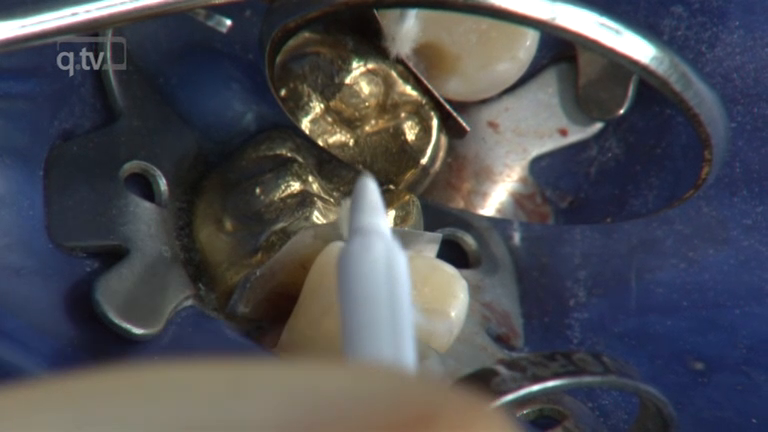
Open Access Online OnlyClinical ResearchDOI: 10.3290/j.jad.c_2106Juni 19, 2025,Seiten: 123-136, Sprache: EnglischMayinger, Felicitas / Lankes, Valerie / Roos, Malgorzata / Rohr, Nadja / Ioannidis, Alexis / Elsayed, Adham / Güth, Jan-Frederik / Edelhoff, Daniel / Passia, Nicole / Esmail, Iman / Beuer, Florian / Wolfart, Stefan / Spies, Benedikt Christopher / Schimmel, Martin / Abou-Ayash, Samir / Hahnel, Sebastian / Schlenz, Maximiliane Amelie / Frankenberger, Roland / Blunck, Uwe / Kraus, Dominik / Engelschalk, Marcus / Huettig, Fabian / Kern, Matthias / Luehrs, Anne-Katrin / Gierthmuehlen, Petra C. / Stawarczyk, BognaPurpose: To investigate, via questionnaire, how protocols for adhesive luting workflows of dental restorations are applied in three German-speaking countries. Material and Methods: A 47-item questionnaire gathered data on airborne particle abrasion (APA) unit characteristics, parameters, operating procedures, pretreatments in adhesive luting workflows for restorations, and participant demographics. The survey was distributed via trade journals, expert associations, universities, technical schools, and social media. Marginal absolute and relative frequencies were analyzed (95% confidence intervals), with Chi-squared tests comparing observed and expected frequencies (P0.05). Twenty-three experts voted on 23 recommendations regarding APA parameters and other pretreatments for bonding restorations. Results: A total of 267 participants completed the survey. Access to an APA unit was linked to a higher likelihood of performing APA before placement. Approximately half of the participants used APA in their practice. For zirconia restorations, 47.2% applied alumina APA at 50 µm/0.1 MPa, while 36.7% used the same settings for polymer-based restorations. For alloys, 37.5% employed 110 µm/0.2 MPa. These preferences correlated with age (≥30 years), experience (≥10 years), profession (dental technician/dentist), prior instruction/training, and daily APA use. Adhesives with MDP were used for zirconia (63.8%) and those with silane for silicate-based ceramics (55.9%). Agreement on recommendations ranged between 52% and 100%, with 21/23 reaching an average of 93%. Conclusion: Access to APA influenced clinical decisions and the feasibility of adhesive luting workflows. Adequate APA equipment in dental facilities is essential for quality care. Standardized protocols, training, and education across dental professions are necessary to enhance understanding and proper use of APA.
Schlagwörter: adhesive dentistry, airborne particle abrasion, parameter, surface conditioning, bonding, dental restoration